Source: PD Dr. Dominik Pförringer
Interview • Drones or data cables?
Are humans too slow for digitalisation?
Today the impressive development of drones by some people is happily regarded as the pinnacle of digitalisation in healthcare. Some groups are testing whether drones can quickly and safely deliver defibrillators to patients in need or whether they can transport laboratory samples or blood products. These developments catch lots of attention, but PD Dr Dominik Pförringer, trauma and orthopaedic surgeon at the Munich University Hospital “rechts der Isar”, is convinced that they ignore the core of the problem: “Drones are not even in the top 100 of my wish list for digital solutions. They are a good tangible example of innovation, however, can serve as an ideal example for the gap between need and demand. Just because an approach is technically possible does not automatically mean it is serving any need or closing an existing gap.”
Interview: Sascha Keutel
Digitization in healthcare resembles teenage sex: 1. Everybody talks about it. 2. Everybody thinks, all others are ahead of them. 3. Nobody knows, how it really works.
PD Dr. Dominik Pförringer
What are the basic needs necessary for a successful digitalisation of hospitals—and what are the main barriers?
Finally, someone asks about the basis instead of the final stage goals. First technical infrastructure is needed that allows fast, secure and efficient—that means frictionless—data exchange. All this requires a budget, which I do not yet see being allocated. Moreover, it is necessary to prepare people for innovation in a structured way and not just send them on an unprepared trip into the future. Specifically, I am talking about continuous education and detailed training. Most physicians, from medical students to the chief physician, harbour resentments based on lack of education and information.
I consider the barriers, surely not insurmountable, to be insufficient extension of data networks, complex data protection laws, which are unspecific and unclear in definition, and the heterogeneous use of technology. While the patient is increasingly open to digitalisation and some practices have progressed, the base is still not properly developed. Wireless communication is lacking as well as soft- and hardware to relieve the healing professions from the bureaucratic burden. For example, most clinics still lack a functioning, comprehensive wireless network to allow secure exchange of medically relevant data.
How does digital technology influence how we offer and deliver healthcare, especially in hospitals?
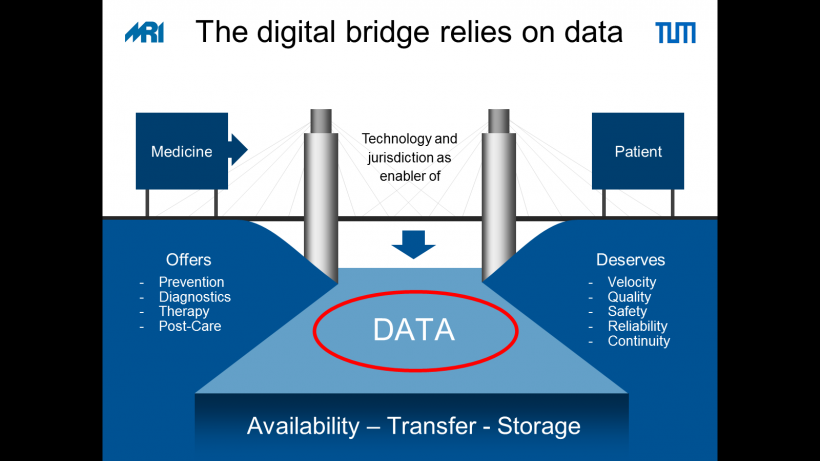
The omnipresence of data makes medicine more complex and at the same time opens a broad field of opportunities, frequently expressed in the cliché, “Data is the oil of the 21st century.” It is often forgotten what this comparison ultimately means: just like crude oil, data per se is of limited use only. The key to success lies in refining the processing of intermediate and final products adding value. If we apply the current technology appropriately to the data (better than now) in the interest of medicine and thus of the patient (again more appropriately than now), then all parties involved can benefit. The patient will gain by obtaining a higher degree of treatment certainty, just as the physician does. More over there is a potential to improve the interface between outpatient and hospital care and as a side effect save costs.

Which digital development will have the greatest impact on the healthcare system?
Generally speaking, digitalisation is not a process with a defined start, never mind a specific end. Digitalisation of healthcare did not begin just yesterday. It is running at full speed and has been for years, however on a relatively heterogeneous scale.
Historically, technology-based subspecialties such as radiology (data imaging) were designed and developed digitally rather early. Other disciplines can learn from these fields. If for example, we apply image and voice recognition intelligently, more time can be used for medicine. I expect the greatest impact from data analysis, data exchange and the resulting process optimisation. The radiology start-up Smart Reporting is working on structured reporting images and constitutes an excellent example of the purposeful application of digital innovation in daily clinical practice.
Can technology improve the quality and performance of medical personnel and the healthcare system?
It definitely can and will, specifically in two ways: physically and cognitively. Take the example of an exoskeleton helping the nurse lift the patient. Or the intelligent nurse paging system like that of the start-up Cliniserve, which helps to bundle activities and thus increase treatment efficiency. The use of artificial intelligence to examine findings can increase precision and thus treatment quality. Caspar Health, a start-up offering digitally based rehabilitation, facilitates the continuous exercise and rehabilitation before and after the patient’s hospitalisation. By means of the specific Better In – Better Out program, treatment procedures can be streamlined, and better results obtained – for the benefit of both patients and therapists
Can medical personnel keep pace with the technological innovation wave?
Human behaviour patterns often resemble the bell curve. A large average does well enough; the long tails comprise on one end, online fans who are technology aficionados and on the other, those who work without any digitalisation at all. The point is to integrate everyone and simplify their use of modern technologies, to lower systematically the so-called “barriers to entry”.
Professor Harald Schmidt predicts the end of medicine, as we know it. Among other things he justifies this with technological progress. Do you agree?
How do we define the end of medicine, as we know it? The interaction between physician and patient has always been the foundation of medicine and that will continue to be the case. Humans need humans to get healthy. Technology helps both sides. They are not a threat but a bridge, an opportunity. Digitalisation will support and complement the physician, but it will never be a replacement. Digitalisation is a tool not a therapy in itself.
Let’s take a look at the future: What will medicine look like in the future?
As an optimist I share and spread a truly positive view of tomorrow’s medicine. Physicians and nurses will be relieved of repetitive, brainless tasks by machines and technologies. The time expended for bureaucratic tasks is finally decreasing after years of continuous growth. Treatment processes can be optimised and accelerated. Let us take the example of prescriptions and compare it to air travel. The share of passengers travelling with a paper ticket has declined to almost nothing. We physicians can learn from that. I look forward to a world in which a prescription is issued digitally and transmitted to the patient who can trigger an order process at his local chemist.
In the end, as always, we physicians ought to define the direction, in fact we must. What does that mean? It is our task to deal with innovation early, to grasp the opportunities, understand the risks and minimise them as well as to recall our Hippocratic oath: to do the best in the interest of the patient and the healing of the patient. Digitalisation can and will help us do exactly that.
Profile:
Priv.-Doz. Dr med habil. Dominik Pförringer studied medicine in Regensburg and earned his doctorate in Munich where he also began his surgical specialist training. Today a specialist for orthopaedics and trauma surgery, he completed the full-time MBA degree at INSEAD in Fontainebleau and Singapore in 2009. In 2010 Pförringer began to work in the healthcare practice of the business consultancy Bain & Company. Since 2013 Dr Pförringer has been working as an orthopaedic and trauma surgeon and DRG officer at the Munich university hospital “rechts der Isar” and acts as an advisor in the fields of venture capital and private equity, as well as the development of digital strategies in healthcare. Dr Pförringer is co-chair of the working group Digitalisation of DGOU (Deutsche Gesellschaft für Orthopädie und Unfallchirurgie).
Event notice:
ETIM 2019 - Artificial Intelligence and Smart Hospital Summit
Saturday, 23 February 2019, 10:00-10:30 am
Digitization of hospitals - Drones or data cables? Where does the deficit pinch?
PD Dr Dominik Pförringer (Munich)
21.02.2019





