Article • The ‘bionic’ radiologist
Three steps towards the future of radiology
Report: Sascha Keutel
Professor Marc Dewey, Vice Chair of the Department of Radiology at Charité – Universitätsmedizin Berlin, made value-based radiology the main theme of the Wilhelm Conrad Röntgen Honorary Lecture during ECR 2018. Radiology practice needs change, he said, and radiologists should grasp at new technology to drive their future. His lecture was summarised in a recent comment in The Lancet.

Dewey’s lecture presented a list of issues regarding current healthcare systems. Among foremost patients’ complaints on hospital admittance is being asked about their medical history multiple times from different staff members or departments. Also, patient care services that decide the clinical strategy and tests to be made have conflicts of interests and different aims. ‘We’re not using evidence-based approaches to make those decisions,’ Dewey said. Additionally, the idiosyncratic terminology in radiologists’ reports prevents major critical findings from being detected. According to Dewey, a recent study on determination and communication of critical findings in abdominal imaging found that one-third of it went undetected (https://www.ncbi.nlm.nih.gov/pubmed/19581643).
A vision of the future
Dewey spoke of a Commonwealth Fund study that concluded that increasing healthcare spending per GDP does not equate to better patient outcomes, or the performance of the healthcare system measured by equity and accessibility. Reality: the more money nations invest in their health care system, the worse the outcome in terms of performance is – a really dramatic result and reason to introduce value-based medicine in radiology, he said. The general goal of value-based radiology is to improve patient outcome with lower cost. ‘Sometimes that means doing less – especially less imaging.’
Value-based radiology, he believes, will gain a central role in addressing three issues:
- Improving personalised decision-making about if, when, and which patients need diagnostic imaging
- Increasing consistency in how images are acquired and interpreted by the ‘bionic’ radiologist
- Enhancing the link on findings and reports with treatment recommendations and management decisions
Source: Dr. Kakuya Kitagawa and Prof. Marc Dewey
Evidence-based decisions
First: Decision support tools, based on evidence, could help to overcome too much imaging in the wrong patients. AI tools would allow better predictions and free up radiologists’ time to talk to a patient. This needs a patient’s data integration with decision support tools, such as the European Society of Radiology’s iGUIDE and eGUIDE.
Second: The integration of AI with human efforts – the ‘bionic radiologist’ – has great potential to increase consistency in radiological image analysis and reduce errors.
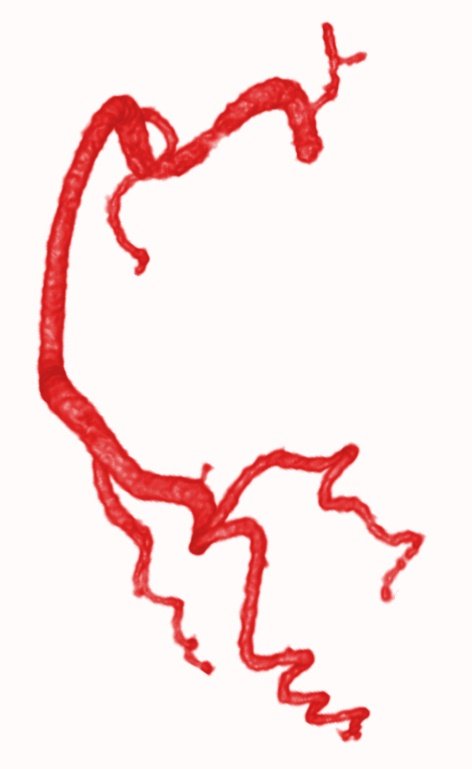
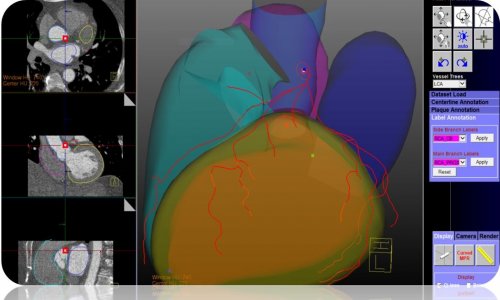
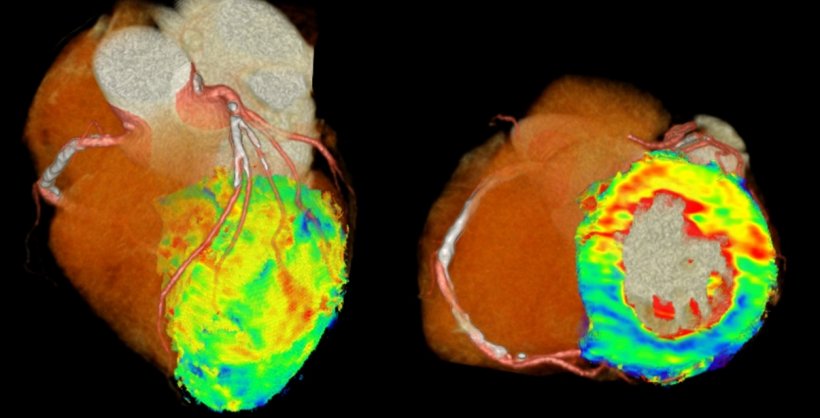
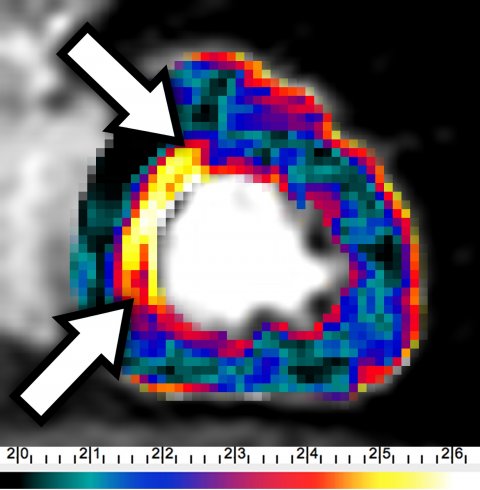
Dewey foresees a human doctor using a device to gain an automated analysis and then interpreting the results and strategies along with a patient. An existing example is 4D-CT of the heart, which produces three billion voxels for a single patient (Figure 1). Patients can’t hold their breath for long, so there’s heart and lungs motion. Can we manually adjust? Can we go through these three billion voxels? That’s very hard to achieve.’ Dewey then explained that radiologists need automated approaches that do registration and pre-processing before a doctor even begins. Figure 2 shows such a pre-processing example of automatic coronary tree segmentation based on 3D cardiac CT.
The bionic radiologist makes use of automated pre-processed data, e.g. using fractal analysis (https://www.ncbi.nlm.nih.gov/pubmed/27436024) while still being the major interpreter and integrator of the data (see Figure 3). This combined approach to leverage both the consistency of automatic analysis and individual interpretation of human image analysis ‘is a paradigm shift,’ Dewey said.
Linking findings to treatment recommendations
Third: Structured reports that combine audio-visual information linked to patient data make them searchable and analysable and therefore improve the reporting, Dewey believes. A study of pancreatic cancer imaging showed that the evaluation greatly improved with structured vs. non-structured reports (https://www.ncbi.nlm.nih.gov/pubmed/25286323). Dewey concludes that structured reporting improves the way radiologists’ discuss a case with referring physicians and plan treatment.
Natural language processing may also help radiologists to avoid a possible culture shock when classic dictation vanishes. While the structure is captured by natural language processing, standardised dictation could continue, he suggests. This would make transition easier because, in the end, ‘culture eats strategy for lunch’.
Challenges and conclusion
Everyone wants to be an innovator, yet no one wants to change
Marc Dewey
‘Everyone wants to be an innovator, yet no one wants to change,’ he said, adding that addressing cultural issues is also important in changing radiologists’ practice. But, for Dewey, the ‘potentially greatest challenge is the half-life of clinical data’. A study on test order prediction tools found that the accuracy of data to predict inpatient orders has a half-life of only four months (https://www.ncbi.nlm.nih.gov/pubmed/28495350). As healthcare changes rapidly, researchers won’t be able to use robust data older than five years. Thus, says Dewey, ‘we don’t need big data; we need good data!’ Success in the three listed areas will free the radiologist to participate more actively in patient care, where automated systems are not good (yet).
Profile:
Marc Dewey is Heisenberg Professor of Radiology, Vice-Chair of Radiology at Charité – Universitätsmedizin Berlin, Germany, and he presided over the Berlin Röntgen Society from 2011 to 2013. He received the Röntgen Award in 2009 and the Curie Ring in 2012 – the German Röntgen Society’s two highest scientific awards. Dewey was also secretary of the 2011 German Röntgen Congress.
25.11.2018