Article • Reducing healthcare costs, optimising patient care
The potential of remote patient monitoring
The remote patient monitoring technology and devices market has attracted significant investment in the past decade and is growing at an extraordinary rate.
Expected to reach around 28 billion euros by the end of 2023, this market is very attractive to many big name companies that want to be ‘connected’ such as Qualcomm Life, Inc., OSI Systems, Inc., Philips Healthcare, Abbott Laboratories and GE Healthcare among others. The promise of reduced healthcare costs while maintaining, or even advancing optimal patient care, being too good to resist. Just how realistic this is and how many healthcare professionals, hospitals and patients are actually using such devices and systems successfully long-term and how much is being saved after initial set up costs is debatable.
3.9 million CVD-related deaths in Europe
Cardiovascular disease (CVD) is the major cause of death for men and women in many European countries. Annually, 3.9 million CVD-related deaths are recorded in Europe – with over 1.8 million in the EU, where, in 2015, around 6.1 million new CVD cases were diagnosed. This means at least 49 million people are living with CVD in the EU alone.
Due partly to lack of awareness in the general population and low rates of diagnosis, these figures are probably underestimated. The absolute number of cases is increasing due to three main factors; poor lifestyle (smoking, obesity, diabetes, lack of exercise), better detection of disease and ageing populations.

The University Hospital Centre (CHU) in Bordeaux, France, realised that a single aspect of CVD, cardiac failure, was seen to account for more than one billion euros expenditure a year, more than 60% of their total budget on hospitalisation for these patients alone. In 2018, Dr Nicolas Pages, a junior hospital doctor in the CHU-Bordeaux was approached by the hospital’s cardiologists for help in reducing this extraordinary burden on their service. Why? Because in 2017, Pages had created the digital start-up Satelia, built on a simple web-based premise. He had shown with a software developer, that it was possible to improve post-operative follow-up of out-patients and reduce associated costs by a simple, user-friendly system.
In this first case, their methodology was based on data gathering by directly interrogating patients to enrich algorithms on post-operative pain. In this way they had, by predictive diagnosis and adjusting prescriptions to individual needs, been able to improve the care for this patient group. And so, the idea of Satelia Cardiologie was born.
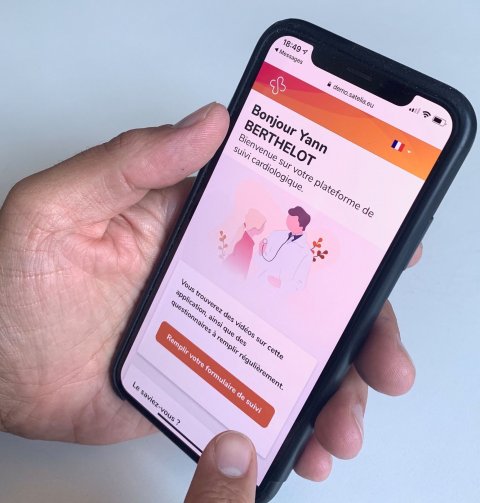
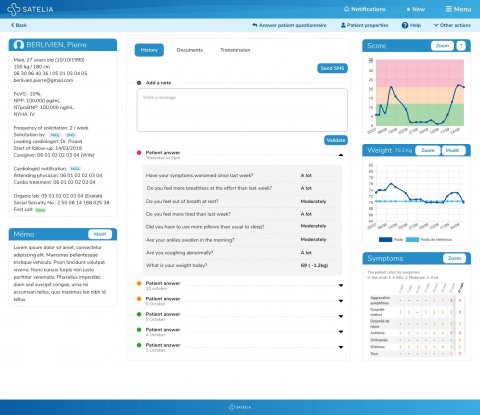
The online-based tool relies on patients entering the system at their primary consultation with the cardiologist. Within a matter of minutes they are registered in the system with a remote connection via their mobile phones or home computers. There is no need to download an application and no special remote monitoring device is required. After the consultation, the patient is sent messages via SMS at the frequency the cardiologist feels is necessary, perhaps once a week, perhaps several times. The messages ask the patient to log-on to the site to fill in a simple questionnaire. Questions are related their symptoms, whether they are out of breath, coughing, more or less tired, have put on weight etc.
Fed into constantly updating algorithms, these data help the cardiologist to assess the patient’s risk level and the need for further consultation, treatment alterations, or an operation. In this way, out-patient appointments are freed up by extending the intervals to see patients whose health is good and disease well-managed, and so allow patients with poorer health, or new patients, to be monitored more closely or to enter the care pathway, respectively.
Online Access
Patients can also access information online about post-operative care and general health from videos specifically targeted to them, based on their questionnaire replies. For those not connected (HF patients tend to be older and therefore some do not have internet access), a nurse will telephone them and fill in the questionnaire for them so that the cardiologist can still follow them remotely and adjust their care accordingly. Since the May 2018 adoption of this system in Bordeaux, admissions for these patients has reduced by 30%.
Designed for simplicity, the system is constantly under development. Pages thinks modifications are requested about 40 times a week, as doctors use and adapt the system. But this doesn’t deter him because it is a clear sign that cardiologists are using the system and seeing where a tweak here or there can make it more accessible and pertinent to their and their patients’ needs. Uptake of the system has been strongly aided by its prescription being 100% reimbursed by social security and by the fact that doctors are at the centre of its development.
Expansion to Italy and Germany
Today, Satelia has 21 employees; including two data scientists and four developers and is ready to expand. Expansion in France has been helped enormously by the reimbursement rate, but Pages also has his sights on Italy and Germany, where he is already working with existing digital platforms that are now licencing Satelia to distribute instead of their own brands, due to its better fit with medical professionals and patients. Satelia, as a concept, can be adapted to remote healthcare anywhere and in any disease.
Pages has plans to cover up to 20 different diseases within the next five to six years and is actively seeking partnerships to develop the system internationally. With such an auspicious start, the world of remote medicine does indeed appear to be Satelia’s oyster.
Profile:
Nicolas Pages MD, a graduate from Bordeaux University, also specialised in emergency anaesthetics, intensive care recovery and paediatric anaesthetics. Currently he works as a medical resident at the Bordeaux University Hospital Centre (CHU). He co-founded Satelia in 2017 and is actively involved in its evolution and development.
23.04.2020











