© Filip Banaovac, MD
Article • Alternative to open surgical procedures gains traction
The future of minimally invasive interventions
In the future, many types of open surgeries will be replaced with minimally invasive interventions, predicts Kevin Cleary, PhD, engineering lead at the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National Hospital, and Professor of Pediatrics and Radiology at George Washington University, both in Washington, D.C. Surgeons and interventional radiologists will be able to plan an intervention, perform it, and immediately verify that it achieved desired treatment goals, he told attendees at the 36th International Conference on Computer-Assisted Radiology and Surgery (CARS2022) held in Tokyo.
Report: Cynthia E. Keen
Minimally invasive surgical techniques limit the size of incisions required, lower associated pain and risk of infection, and reduce the time for the wound to heal. Minimally invasive interventions include non-surgical procedures, such as high-intensity focused ultrasound (HIFU), which is used to destroy targeted tissue using heat from sound waves instead of surgical resection. At Children’s National Hospital, HIFU is used to treat osteoid osteomas, painful benign bone tumours.
Medical robotics technology was first implemented in 1985, for neurosurgery drilling. Dr Cleary explained that the three classes of medical robots used today are:
- tele-operated, a “master-slave” configuration in which a surgeon sits at a master console and controls a slave robot (e.g., the DaVinci Surgical System);
- cooperative, a robotic system that works synergistically with a surgeon (e.g., Mako SmartRobotics, Stryker) to constrain the cutting plane during knee osteotomy); and
- preprogrammed, a robotic system that executes a pre-programmed plan based on segmentation of medical images (e.g., Cyberknife System, Accuray, for stereotactic radiosurgery).
Image-guided navigation systems also enable minimally invasive interventions. These systems consist of a computer for control and display, a localizer for electromagnetic tracking of instruments, and software for image processing.
© Yue Chen, PhD, Georgia Institute of Technology
Robotics and MRI – a winning combination
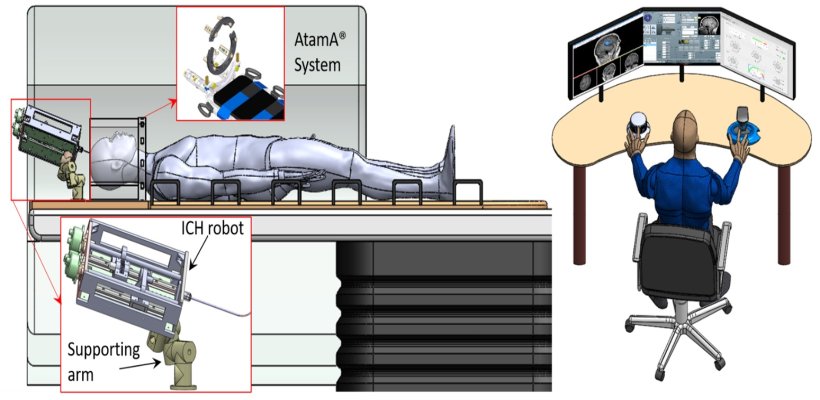
MRI compatible robotics for in-bore interventions are currently under development. These include systems for shoulder arthrography, back pain diagnosis, long bone biopsy, and intracerebral haemorrhage. ‘People question why an expensive MRI scanner would be used for minimally invasive interventions, but the images provide exquisite soft tissue discrimination, MRI does not expose a patient to radiation, and other functionality such as monitoring of thermal treatment can be provided,’ said Dr Cleary. ‘MRI compatible robotics are not hindered by difficult access in a closed-bore MRI, and can enable in-bore interventions that a surgeon logistically would not be able to do. Robots can provide a steady guide for instrumentation, facilitated by real-time MRI guidance.’
Surgical technology is rapidly improving, driven in part by advances in the consumer market, such as high-resolution displays, the rise of artificial intelligence, and new user interfaces
Kevin Cleary
‘Many challenges need to be overcome,’ he added. ‘The development of dedicated high quality robotic systems requires the synthesis of mechanical design, electronics, computer science, and control. The strong static and switching magnetic fields and radio frequency pulses used in MRI create a safety hazard and compatibility issues. These exclude the use of conventional robotic technology. It will require clinicians and equipment designers to work together.’
‘Medical robotics has the potential to enable new minimally invasive interventions by providing a surgeon the ability to access the anatomy through smaller incisions and in a more dexterous manner than can be done with conventional laparoscopic instruments. Surgical technology is rapidly improving, driven in part by advances in the consumer market, such as high-resolution displays, the rise of artificial intelligence, and new user interfaces,’ he said.
Open exchange to promote cross-system compatibility
‘The challenge in integrating consumer-driven advances in an operating room suite includes integration issues that may arise when combining products from different vendors. The regulatory environment requires each individual device to be approved. If devices are to be used as part of an integrated system, the system needs to be evaluated and approved to ensure that it is safe to combine devices. The advantage to the surgeon of such a systems approach would be that a single user interface might be created to operate multiple different devices which would be more user friendly.
‘CARS can help make this happen, because it is focused on bringing engineers, scientists, and clinicians together to develop the next generation of medical technology. This annual conference promotes open exchange and sharing of information. It is continuously evolving to reflect the latest developments in the field,’ concluded Dr Cleary.
Profile:
Kevin Cleary, PhD, is the technical director of the bioengineering initiative of the Medical Robotics Laboratory of the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National Hospital in Washington, D.C. This research group focuses on developing novel biomedical devices to improve the health and care of children. Its research areas include medical robotics, medical devices and mobile apps. Dr. Cleary is also Professor of Pediatrics and Radiology at George Washington University.
11.10.2022