Article • Cardiology
‘The future belongs to the heart team’
A formerly bitter competition between cardiology and cardiac surgery is increasingly replaced by constructive cooperation. The Austrian Society of Cardiology (ÖKG) even held its annual congress along with the Austrian Society of Thoracic and Cardiovascular Surgery this year.
Report: Michael Kraßnitzer

‘There should be no competition between the two different disciplines; to the contrary, the entire heart team needs to find appropriate solutions for individual patients,’ emphasises Franz Xaver Roithinger MD, President of the ÖKG. ‘The future belongs to the heart team.’
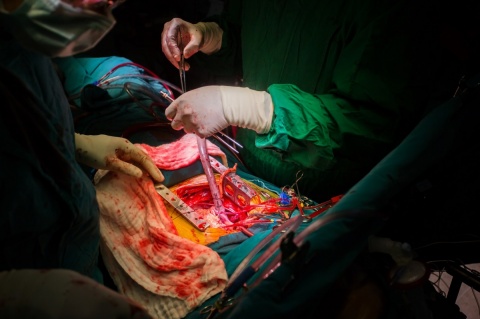
These multi-professional teams include cardiologists, cardiac surgeons and other specialists, such as anaesthetists if required, who make the relevant treatment decisions together - decisions such as whether a patient should undergo open heart surgery supported by a heart-lung machine or whether they should receive less invasive treatment using cardiac catheterisation. ‘The lines are already a little blurred,’ Roithinger explains. ‘Minimally invasive procedures are increasingly used in heart surgery whilst there are catheter interventions that involve the heart being tapped.’
Both disciplines offer different solutions for numerous problems. In interventional cardiology, blocked coronary vessels, for instance, are treated with stents that are inserted via cardiac catheters and moved into the required position in previously dilated vessels. Heart surgery solves this problem with bypass surgery. The occluded vessel is bypassed with a venous graft taken from a patient’s leg. ‘Both procedures have their special features, advantages and disadvantages. The heart team discusses these cases and selects the best solution for each individual patient,’ Roithinger points out.
Patients with several coronary occlusions, who would alternatively require the insertion of numerous stents to ensure adequate blood supply to the heart, are typical candidates for bypass surgery. ‘Studies have also shown that diabetics with heart disease experience more benefits from bypass surgery than from the insertion of stents,’ he adds. ‘In contrast, the stent is preferable for all patients who do not suffer from any other complications because the implantation is significantly less invasive than heart surgery.’ Implantation of artificial heart valves, particularly aortic valves, is a further interface between interventional cardiology and heart surgery. For some years transcatheter aortic valve implantation (TAVI) has been an increasingly popular alternative to heart valve surgery.
Inoperable or high risk cases benefit from TAVI
‘TAVI is now an established procedure to treat aortic valve stenosis for inoperable patients and particularly high risk patients,’ Roithinger says. ‘According to figures from the AQUA register (the German Institute for Applied Quality Improvement and Research in Health Care GmbH), TAVI also has a lower mortality risk than conventional surgery for patients at medium risk. However, whether TAVI should generally be recommended for medium risk patients needs to be confirmed by large-scale, randomised studies.’
This is another area where the heart team seeks the right solution for individual patients. Roithinger banks on the rule of thumb: Older patients and patients in worse health are more likely to be treated with TAVI to avoid the risks of open heart surgery. Younger, healthier patients are more likely to undergo heart valve surgery because they can still anticipate a longer life expectancy and because there is no long-term data available on TAVI yet. ‘However, Roithinger pointed out, ‘the heart valves implanted via TAVI are increasingly more durable so,’ he adds, ‘in all likelihood, the procedure will also see more use for younger patients in future.’
28.08.2017





