Teleradiology use in Europe
A new survey brings fresh insight into radiologists’ thoughts on teleradiology in Europe. Conducted by radiologist Dr Erik Ranschaert from the Jeroen Bosch Hospital, Den Bosch, The Netherlands, the findings were presented in March to a Special Focus Session at the European Congress of Radiology in Vienna. Mark Nicholls reports.


The Radiology on the road: Working when you are away from home ECR 21012 session examined challenges and opportunities posed by teleradiology, the use of hand held devices, portable reporting and legal issues. A question posed by Dr Erik Ranschaert -- Teleradiology in 2012: growing or shrinking in importance? – presented findings from his European Teleradiology Survey, which looked at the issues, challenges, driving factors and future of teleradiology in Europe and beyond.
The aim of the online survey – with 32 multiple choice and three open questions - was to map current use of teleradiology in Europe, he said, and to examine the potential and appetite for further implementation of teleradiology services in Europe. Among the 368 participants from 35 different countries, the largest responses came from Belgium, Austria, UK and The Netherlands. The data revealed that teleradiology is used by 65% of respondents either in institutions or at home, for second opinion requests and to transfer images to a company or academic centres for research purposes. When quizzed about the advantages of teleradiology, the most important aspects from respondents was the chance to collaborate, ability to sub specialise and as a way to improve efficiency.
Outsourcing was used by 35% of respondents (49% of those as part of their regular workflow and 42% for second or expert opinions) and of the work outsourced, 52% went to a commercial provider within their own country, 32% to a tertiary centre and 13% to a provider in the EU with the remainder going elsewhere. Dr Ranschaert said outsourcing also solved temporary capacity problems, though some people were concerned the quality of reports would be reduced. Asked what could improve teleradiology, 81% said clear national and EU legislation covering teleradiology was needed, while 78% felt there should be an obligatory quality assurance system in place. But, he added: ‘80% had a positive or strongly positive opinion about teleradiology and 46% think its importance will grow, while 20% maintain the need for better standards and better financial and legal controls.’
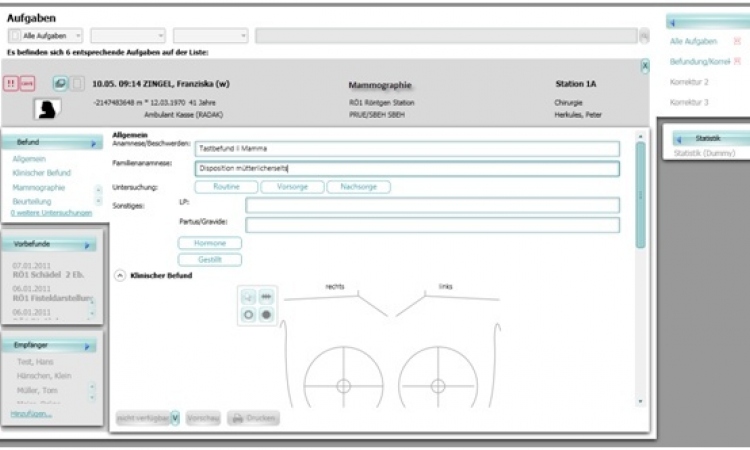
Key reasons to develop future teleradiology, according to respondents, are the shortage of radiologists, the need for specialist advice and need for on-call reading. Increasing healthcare costs and decreasing budgets also see teleradiology perceived as a ‘relatively cost effective solution’. While demand and PACS availability was a driving factor for teleradiology, there is variation in PACS across Europe. Nordic countries have 100% availability, with the UK close behind, while France and Greece only have PACS coverage of 25%, which makes teleradiology difficult, he said.
In the EU, most teleradiology is in-house or within an institution and amounts only to 2% of all procedures – with the UK and Germany the biggest users - compared to 20% in the US . Dr Ranschaert concluded: ‘Teleradiology is likely to be an integral part of healthcare delivery across Europe and its impact will definitely increase but there are still key issues to be solved about cross border use, security, quality assurance and financial flexibility and with language there needs to be more semantic interoperability between countries. ‘There is still a need for a quality framework and, from a legal point of view, there should be uniform European legislation with regard to teleradiology.’
The survey was conducted with the support of the European Society of Radiology and full results will be published in the near future. During the session, Professor Osman Ratib from the Department of Medical Imaging and Information Sciences, University of Geneva, Switzerland, examined the use of PDAs (Personal Digital Assistants) and other hand held devices in radiology. The medical field quickly adopted new handheld technologies and, he predicts, there will be higher resolution images available in small format and a greater use of portable devices in a clinical environment, such as surgeons taking their iPads into the operating theatre as part of standard theatre equipment.
Consultant radiologist Dr Richard FitzGerald, from the Royal Wolverhampton Hospitals NHS Trust, said there remained issues over the regulation of teleradiologists and, he added: ‘We should not just be concerned with cross border regulation in Europe but also take in the global perspective. My advice to radiologists is not to let standards slip when using mobile devices and check your indemnity cover if doing teleradiology, particularly if reporting in another country.’
06.06.2012