Sprayed on skin
Although scientists and medics have sought ways to grow artificial skin in laboratories since the 1970s, only now has it become possible to reproduce the top layer of skin, thanks to work at the Trauma Surgery and Orthopaedics Clinic in Berlin (ukb).


The young woman had been holding a bottle of barbecue lighter fuel in her hand when it suddenly burst into flames. With large-scale burns to the face and hands, she needed skin grafts. The patient was admitted to the ukb Burns Unit -- one of the largest and most modern facilities of its kind in Europe. There she is to benefit from results of the work of doctors at the Trauma Surgery and Orthopaedics Clinic in Berlin (ukb), a team that is also involved in the EuroSkinGraft project with researchers from Switzerland and the Netherlands. Their joint efforts aims to recreate multi-layer skin to improve grafts. For a decade, consultant Dr Bernd Hartmann and team at the Severe Burns and Plastic Surgery Centre (BVZ) have worked on artificial skin graft development, finally arriving at a spray-on skin that promises to heal second-degree burns without scarring. This product is now ready for mass production.
One step removal and re-spraying
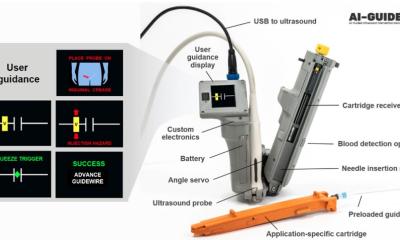
The human skin, our largest organ, protects against cold, heat and even viruses. Many small skin injuries heal by themselves. However, the destruction of large areas and several layers of skin is critical All procedures for growing artificial skin utilise the patient’s remaining, healthy skin. Initially an area of skin the size of a postage stamp is removed from an affected patient and these cells are usually cultivated in laboratories and grown for a few days. The new spray-on skin from Berlin shortens that process: From the patch of healthy skin, cells are extracted enzymatically, put in an electrolyte solution and then resprayed an hour or two later, in a sterile operating theatre. Dr Hartmann: ‘We call this a “one-time” procedure because the skin cells are removed and replaced within the same operation. We basically intensify the healing process. The important cell growth occurs directly in the wound.’
Utilising the wound healing mechanism
The ukb procedure – from removal to application via spray can – has not only been largely standardised but also, adds Dr Hartmann of its particular success ‘… our spraying of skin cells almost always ensures wounds heal well or very well whilst avoiding scarring.’ The specialists utilise the body’s natural mechanisms and literally trick them. ‘The body’s additional skin cells speed up the wound healing. This in turns stops the process of scarring.’ When the barbecue victim underwent the procedure about ten days after the accident, her skin cells were removed, cultivated in a suspension and transplanted as a solution via the spray gun a few hours later. Led by Professor Axel Ekkernkamp, Medical Director of the ukb, the supra-regional Trauma Centre, is currently planning to equip other large German Burns Units with the necessary technology and training for skin cell spray transplants. In partnership is the German Institute for Cell and Tissue Replacement (DIZG) in Berlin, the country’s only organisation licensed to grow artificial skin from the body’s own tissue. Although the skin cell spray solution is impressively simple, numerous problems associated with artificial skin replacements remain unresolved due to the skin’s complex, three-layer structure. The lower layers are particularly important for the human organism; they contain the lymphatic and blood vessels as well as immunological cells. For very deep burns the skin cell spray application does not suffice.
EuroSkinGraft
Could a multi-layer skin replacement be developed quickly? Solving that need for the benefit of accident victims is the EuroSkinGraft project’s objective and it is this on which Dr Hartmann and his Swiss and Dutch colleagues are focused. Coordinating the project is PD Dr Ernst Reichmann, at the University of Zurich, who heads the Surgical Clinic research division and has been involved in developing and testing clinically usable, complete skinreplacement for years. Within the project, Professor Esther Middelkoop MD, from the Medical Centre at the University of Amsterdam, is a skin wound healing expert. Dr Hartmann’s ukb patients will be the first in Germany to benefit from these new procedures. Expected to last five-years, the project is subsidised by just under €6 million from the EU. Many regulatory obstacles must still be overcome. Legally in Europe artificial skin is classed as a pharmacological substance. Therefore, growing tissue outside the body under the terms of the Pharmaceuticals Act requires licensing. The complex project management is overseen by Gabo:mi in Munich, which assists organisations with applications for and the execution of scientific projects, particularly in the healthcare sector.
04.09.2012