© Gorodenkoff – stock.adobe.com
Article • Overheard at Semi-Live 2024
Exchanging insights on advances in urological surgery
The sixth Semi-Live event took place at University Hospital Heidelberg, the very same location it was initially held in 2015. The host, Professor Dr. Markus Hohenfellner, Chairman of the Department of Urology at University Hospital Heidelberg, told the audience that the idea for the event ‘was born by dreaming’. It came to life after he had secured the support of Dr. Sybill Storz, at the time Chief Executive of Karl Storz, a medical equipment manufacturer of endoscopy instruments, and Patron to the Royal College of Surgeons in England.
Report: Cornelia Wels-Maug
Since its inauguration, Semi-Live has developed into an internationally renowned conference format that serves as a platform for exchanging experiences amongst urologists in the form of presentations, video footage from surgeries or live transmissions from operating theatres. For Hohenfellner, surgical techniques constitute the cornerstone of urology. They are deployed for oncological operations, reconstruction, benign prostatic hyperplasia (BPH), benign prostatic obstruction (BPO), kidney transplantation, and kidney stone removal, to name but a few pathologies.
Surgeons can choose from a variety of surgical approaches including open surgery, laparoscopy, shock waves as well as robotic, endourological and microscopic procedures. Since a multitude of urological indications can be treated with various procedures that lead to comparable outcomes, an event where urologists from across the globe share their experiences with diverse treatment options is especially valuable and relevant. Discussions at Semi-Live made it evident that there are not only individual preferences in surgical approaches, but also national preferences.
The advancement of urology
The conference looked at how surgical approaches have evolved in the last few decades driven by technical advances in the ongoing quest for precision and excellence in patient care. Here are exemplary insights from selected speakers:
Dr. Viktoria Schütz, Department of Urology, University Hospital Heidelberg, Germany, dedicated her presentation to the evolution of salvage prostatectomy. She pointed out that advances in surgical techniques led to an evolution in salvage prostatectomy that resulted in reduced peri-operative and postoperative morbidity. However, Schütz made clear that salvage surgery is more demanding and is associated with higher risks to other organs, especially the rectum.
Prof. Dr. Lukas Lusardi, Chairman Department of Urology, Paracelsus Medical University Hospital, Salzburg, Austria, compared transurethral resection of the prostate (TURP) to minimal invasive alternatives in his presentation. Compared to newer bladder pain symptoms (BPS) therapies, TURP can look back on decades of documentation. The reintervention rate after TURP due to a BPS recurrence after 8 to 22 years lies between 1.9% and 7.4% and 79% of patients are still satisfied with the results of the TURP intervention more than 15 years later. Lusardi explored minimal invasive alternatives to TURP, including Urolift, iTind Prostatic Artery Embolization (PAE) and Rezum. PAE is less effective than TURP at improving symptoms and urodynamic parameters such as flow rate and needs a longer procedural time but scores higher than TURF with regards to blood loss, catheterisation and hospitalisation time. Nevertheless, it can be performed under local anaesthesia.
No need for nostalgia
Associate Prof. Dr. Jörn H. Witt, Head of Robotic Urology, Goldstadt Clinic, Pforzheim, Germany, discussed newer surgical approaches to what he referred to as the “open days”: these were characterized by high blood loss, up to six catheters, stents or drains, lengthy hospital stays and catheterization, accompanied by high stricture and complication rates in addition to a prolonged general and functional recovery period. He reviewed the performance of open surgery and minimal invasive approaches – endoscopic, laparoscopy and robot-assisted surgery – when measured against 3D vision, degrees of freedom, option for complex movements and the spectrum of magnification.
Robot-assisted surgery clearly outperformed all other approaches in terms of magnification rate (10-20 times). In his view, robot-assisted surgery is in many aspects closer to open surgery than to laparoscopy. Witt advised that in the end, the oncological and functional results of surgery depend on an individual’s anatomical understanding, tissue handling and experience, in addition to a surgeon’s talent, training, reflection and retraining and team factors including communication skills. He ended with an appeal to practice critical thinking and keep learning: ‘A lot of things we can still do better.’
Dr. Karin Lehrich, Urological Laser Center, Vivantes Auguste-Viktoria-Hospital, Berlin, Germany, demonstrated how to master the Holmium Laser Enucleation of the Prostate (HoLEP) technique. Starting with endourological experience and knowledge of anatomy and physical laser characteristics, she delved into the importance of teaching and coaching, including the attendance of workshops and webinars, visiting excellence centres and having a mentor as well as supervision. Lehrich also recommended simulator and hand-to-hand training, as well as studying video clips and YouTube for mastering laser physics. She explained the intricacies of laser-tissue interaction, urging surgeons to understand the ideal distance between the laser fiber tip and the tissue for optimal outcomes.
Regardless of the chosen approach, Hohenfellner urged surgeons to keep self-assessment as a fixed part of their daily routine: ‘We need to establish if we are fit to do what we want to do’, he said.

Photo: Cornelia Wels-Maug
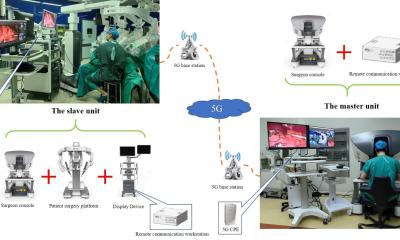
Telesurgery in action
True to its name, Semi-Live featured several live demonstrations of telesurgery. In one case, Prof. Xu Zhang, head of the urology department at the People’s Liberation Army General Hospital, Beijing, China, performed a radical prostatectomy. Zhang, who has spearheaded robot-assisted laparoscopic surgery in China, has also pioneered remote and intelligent surgery. In the televised live remote prostatectomy, he used edge robots with a resolution of 1080 pixels to operate on a patient located in Sanya, a Chinese city 3,000 kilometres south of Beijing. China Telecom provided an Optical Transport Network (OTN) to enable the high-speed data transmission, whereby the surgery was performed using a dedicated line with a bandwidth of 60 MHz. The delay of 117 milliseconds remained unnoticed by the surgeon, however, a delay larger than 200 milliseconds would be noticeable. A doctor of Zhan’s team who was present in the audience in Heidelberg explained that there was also a surgical team standing by at the patient’s side in Sanya so that they could carry on with the operation in case transmission problems would occur.
A glimpse into the future of surgery
Will robots take over in the operation theatre? When Hohenfellner turned to ChatGPT for an answer, he was told by the chatbot that it was quite conceivable that AI-based “large motor models” could be developed in the future. These might perform fine motor tasks, with a focus on the physical interaction and manipulation of objects by robots. Possible applications of such models could be in surgery or other areas where precision is critical. It will be left to future Semi-Live events to explore this topic further.
17.10.2024