News • Cerebral venous sinus thrombosis
New score to predict epilepsy after CVT stroke
Researchers from 15 countries, led by Amsterdam UMC, have developed a way to predict which patients are at risk of epilepsy after a cerebral venous sinus thrombosis (CVT).
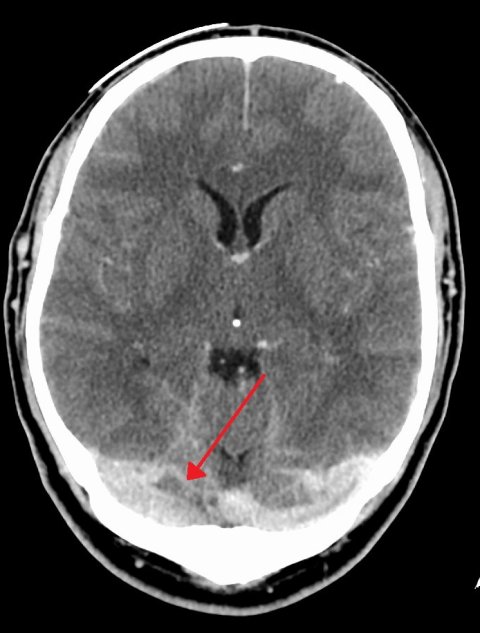
Image source: James Heilman, MD, Duralvenoussinusthrombosis, CC BY-SA 4.0
CVT is a type of stroke that typically affects women between the ages of 20 and 50. The prediction model is now available worldwide free of charge and research it is based on is published in JAMA Neurology. "We hope that as many physicians as possible will use this score to better treat and educate CVT patients across the world," says lead researcher and neurologist at Amsterdam UMC, Jonathan Coutinho.
CVT occurs when a clot blocks the veins that drain blood from the brain, preventing blood from draining properly. In the Netherlands, it affects 250 people every year, three-quarters of whom are women, occurring mainly in younger people, between 20 and 50 years old. One in ten of these patients develops epilepsy after the stroke, often months later, as a result of the damage to their brain damage. "These patients usually have to take medication for life and epilepsy has, naturally, a negative impact on their quality of life. Until now, it was not possible to predict which patients have the highest risk of developing epilepsy after sinus thrombosis," says Coutinho.
Because it mainly affects women at an age when they are in the middle of their careers and maybe starting a family, it is important for them to know if they should take epilepsy into account
Jonathan Coutinho
Due to the relative rarity of the disease, it is difficult to collect data from a sufficient number of patients. The Amsterdam UMC team therefore collaborated with researchers from 15 countries, including more than 10 centres in the United States. Together, they analysed data from over 2,000 patients from 1994 to 2022, focusing on data from patients who developed epilepsy between 7 days and 3 years after their stroke.
By predicting which patients are at a greater risk of developing epilepsy, healthcare professionals also learn which patients are likely to need epilepsy medication in the long term. This facilitates the development of personalised treatment plans and allows the treatment team to prepare the patient for possible epileptic seizures in the future. The patient can then take precautions, for example by no longer driving a car.
"Because it mainly affects women at an age when they are in the middle of their careers and maybe starting a family, it is important for them to know if they should take epilepsy into account," explains Coutinho. "We hope that this score will also help healthcare providers in the guidance of CVT patients and that it will contribute to follow-up research into treatment with anti-seizure medication. Ultimately, we want to completely prevent epilepsy after CVT," he adds. This research and the worldwide online availability of the prediction model show the power of international academic collaboration, especially in rare diseases where there are few patients per country.
How does the DIAS3 scoring prediction model work?
On the basis of 6 indicators, it is possible to predict the risk of epilepsy in an individual patient after this type of stroke. These data are already routinely collected in patients with CVT. The 6 indicators used in the model are:
- age,
- a cerebral haemorrhage,
- seizures in the first 7 days,
- status epilepticus (epileptic seizure that does not stop on its own) in the first 7 days,
- subdural hematoma (haemorrhage between the outer two membranes of the brain) and
- a surgical procedure in which the skull is (partially) lifted to prevent swelling of the brain.
With these data, the computational model can predict each individual patient's risk of epilepsy.
Source: Amsterdam University Medical Center
24.10.2024