News • Biomedical project
Saving hearts after a heart attack
University of Alabama at Birmingham biomedical engineers report a significant advance in efforts to repair a damaged heart after a heart attack, using grafted heart-muscle cells to create a repair patch. The key was overexpressing a gene that activates the cell-cycle of the grafted muscle cells, so they grow and divide more than control grafted cells. Up to now, an extremely low amount of engraftment of cardiomyocytes has been a stumbling block in hopes to use grafted cells to repair hearts after a heart attack. Without the successful repair that a graft could potentially offer, the damaged heart is prone to later heart failure and patient death.
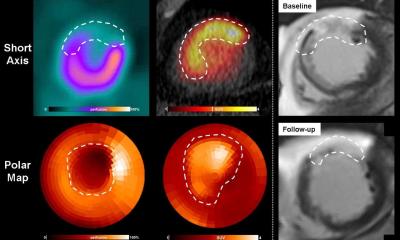
In experiments in a mouse model, UAB researchers showed that gene overexpression of the cell-cycle activator CCND2 increased the proliferation of grafted cardiomyocytes. This led to increased remuscularization of the heart at the dead-tissue site of the heart attack, a larger graft size, improved cardiac function and decreased size of the dead tissue, or infarct.
Besides regenerating muscle, the grafted cells also increased new blood vessel formation at the border zone of the infarct, apparently through increased activation of the paracrine mechanism. The UAB team used cardiomyocytes that were derived from human induced pluripotent stem cells, as they work toward a goal of eventual clinical treatment for human heart attack patients. This UAB study, published online in Circulation Research, is led by Jianyi “Jay” Zhang, M.D., Ph.D., chair and professor of the UAB Department of Biomedical Engineering and holder of the T. Michael and Gillian Goodrich Endowed Chair of Engineering Leadership.
Study details
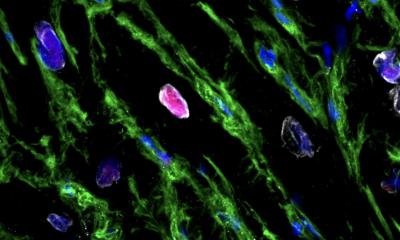
Researchers first showed that overexpression of CCND2 in the human induced pluripotent stem cells-derived cardiomyocytes, or hiPSC-CMs, increased the proportion of cells that exhibited markers for the S and M phases of the cell-cycle, and for cytokinesis, as measured in cell culture. When they injected overexpressing hiPSC-CMs into the infarct region and the border of the infarct in the mouse model, the left ventricle ejection fraction was significantly greater at week four and the infarct size was significantly smaller, as compared with mice receiving normal hiPSC-CMs that did not overexpress CCND2. Both treatments were improvements as compared with untreated mice.
Overexpression also led to an increased number of engrafted hiPSC-CMs, as measured by bioluminescence and human cell markers.This appeared to be due to proliferation of the cells because both the number and proportion of overexpressing hiPSC-CMs increased from week one to week four, and the human cells engrafted in the heart tissue expressed markers for the S and M phases of the cell-cycle, and for cytokinesis.
Co-authors with Zhang of the study, “CCND2 overexpression enhances the regenerative potency of human induced pluripotent stem cell-derived cardiomyocytes: Remuscularization of injured ventricle,” are Wuqiang Zhu, Meng Zhao, Saidulu Mattapally, UAB Department of Biomedical Engineering, a joint department of the UAB School of Medicine and School of Engineering; and Sifeng Chen, Fudan University, Shanghai, China.
Source: University of Alabama
18.10.2017