Robot-assisted total knee replacement
By Professor Werner Siebert, head of the Kassel Orthopaedic Centre, assisting surgeon Dr Sabine Mai, Dr Rudolf Kober, Chief Technology Officer at URS-ortho GmbH, and Dr Peter Heeckt, Medical Director at Fresenius ProServe
Total knee replacement (TKR) is a common procedure for treatment of severe gonarthrosis, but the outcome may be unsatisfactory due to primary malalignment of the prosthetic components. To improve precision and accuracy of this surgical procedure, CASPAR, a commercial robotic surgical system, has been adapted to assist the surgeon in preoperative planning and intraoperative execution of TKR

So far, 70 patients with idiopathic gonarthrosis were successfully treated with robot-assisted technique in our institution. No major adverse events related to the use of the robotic system have been observed. The mean difference between preoperatively planned and postoperatively achieved tibiofemoral alignment was 0.8º (0-4.1º) in the robotic group versus 2.6º (0-7º) in a manually operated historical control group of 50 patients. Clear advantage of robot-assisted TKR seems to be the ability to execute a highly precise preoperative plan based on computed tomography (CT) scans. Due to better alignment of the prosthetic components and improved bone-implant fit, implant loosening is anticipated to be diminished, which may be most evident in non-cemented prostheses. Current disadvantages, such as the need for placement of fiducial markers, increased operating times and higher overall costs have to be resolved for the future.
Surgical technique
Placement of fiducial markers
To facilitate orientation, the robot requires placement of a femoral and a tibial pin that serve as fiducial markers. The pin design is a self-tapping bone screw to which a special CT cross can be affixed. This will be detected by later computed tomography. The pins are placed into the femur by an anterior approach and into the tibia via an anteromedial approach (figures 1+2). The stab incisions are positioned in such a way that they can later be incorporated into the primary surgical incision. The robot uses these pins for spatial orientation and performs geometric calculations based on their location. To maintain the pins in the required stable position, they are placed bicortically. The incisions are closed over the pins and the main procedure is performed on the same or on the following day. Placement of both pins takes about 15 minutes on average. Major problems or complications were never encountered during the pin placement procedure. No stress fractures at the pin sites were observed in the follow-up period.
CT-scan and preoperative planning
A helical CT scan is obtained immediately after the pins have been placed. Particular attention is paid to the areas of the femoral head, pins, knee and ankle. A calibration rod is placed next to the extremity. The rod helps to control the CT scan quality, in terms of motion artefacts. The average time for the preoperative CT scan is 15-20 minutes. During imaging, our patients are maintained under a spinal or epidural anaesthesia from the pin placement procedure, greatly reducing the risk for motion artefacts. However, if the CT unit is too far from the operating room the CT scan can certainly be taken at any later time without anaesthesia.
The CT data are then transferred into the PC-based planning station. The scan’s technical quality is automatically checked and the pin position verified. The surgeon identifies specific anatomical landmarks and the anatomical and mechanical axes of the femur and tibia are calculated in the frontal and sagittal planes. The joint line, epicondylar twist (angle between epicondylar line and posterior condylar line), torsion of the tibia (angle between dorsal part of the tibial plateau and a line through the centre of the ankle), as well as the relationship of the dorsal part of the tibia and the condylar line, serve as additional important parameters. All angles and possible geometric translations are displayed on the video screen at the end of the planning procedure (figure 3).
The system allows the user to select and position a specific implant size. One needs to decide on the required degree of femoral and tibial external rotation to assure central patellar tracking. Either a classical or anatomical joint line plus the amount of dorsal slope may be selected. Unintentional notching can easily be avoided. With computer-assisted planning, the strong interdependence of all parameters, including the mechanical axes, becomes quite evident. Implant fit can be accurately assessed by scrolling through the scan - a feature that sometimes makes the surgeon ‘pickier’ regarding selection of a specific implant type or size. The system informs the user about the expected change in ‘extension’ and ‘flexion gaps’ and the resulting ligament tension. This feature of the planning software enables the surgeon to anticipate the amount of intraoperative soft tissue balancing.
After positioning the implants, it is important to specify the milling areas, to avoid redundant cutting and to protect surrounding soft-tissue. As a last step, the system prints out an overview of the final plan. All data are stored on a PC card and transferred to the robot control unit immediately before surgery. After an initial learning period the preoperative planning procedure requires about 15 minutes.
Robot-assisted surgery
A conventional median incision with parapatellar approach to the knee joint is used. The knee joint is secured by a transfemoral and transtibial self-cutting screw to a specially designed frame. This rigid frame is also used for fixation of self-holding soft-tissue retractors. Sufficient mobility to allow 50 ipsilateral hip flexion is a prerequisite for securing the leg in the fixation frame. Intraoperative difficulties can be caused by a very tight quadriceps muscle or patellar tendon.
Since it is necessary to provide sufficient lateral traction on the patella to keep it out of the way when milling the tibial plateau, a temporary release of the tibial tuberosity or a ‘quadriceps snip’ may be required in very rare instances. To control for unwanted leg micro-movements during robotic surgery, rigid bodies with reflective spheres are firmly attached to the frame. The passive markers are constantly monitored by an infrared camera system, which will automatically shut off the robot in the event of excessive motion.).
After registration of the fiducial markers, robotic milling is started by the surgeon. As a safety measure, the surgeon must constantly depress the robot button on a sterile remote control, to maintain the cutting action. The cutting tool is equipped with internal water-cooling and irrigation. A splash-guard helps to keep the operative field and reflective spheres dry and clean. Milling heads are changed during the procedure depending on the type of cut to be made. Varying with the size of the implant and bone density, the entire milling procedure takes approximately 18 minutes. If required, it is possible to revert to conventional manual technique at any point during surgery.
The resulting bone surfaces are accurately shaped and smooth. After the fixation frame and pins are removed, soft tissues are balanced in the classic technique, according to the preoperative plan. The components of the implant are then inserted.
First clinical results - After a developmental phase in 1999 and a series of successful experiments on phantoms and cadaver bones, a prospective clinical study was started in March 2000 at the Kassel Orthopaedic Clinic.
The first clinical robot-assisted TKR was performed on 27 March 2000. Since then, 70 robot-assisted TKR’s have been performed in 69 patients (48 women, 21 men). One female patient received simultaneous, bilateral TKR. The average age in the robotic group was 66 years (46-87 years). The manually operated historic control group consisted of 52 patients (40 women, 12 men) - average age 68 years (48-82). The indication for TKR was idiopathic gonarthrosis in all cases. The LC Search Evolution knee-system (Aesculap, Tuttlingen, Germany) was used for all patients in the robotic group, because this was the first knee implant system geometry that was loaded into the planning software. All patients in the historic manual control group received NexGen (Zimmer Inc, Warsaw, Indiana, USA) implants.
All complications during surgery and in the postoperative course were recorded. Patients were scored before and after surgery according to the Knee Society Score.
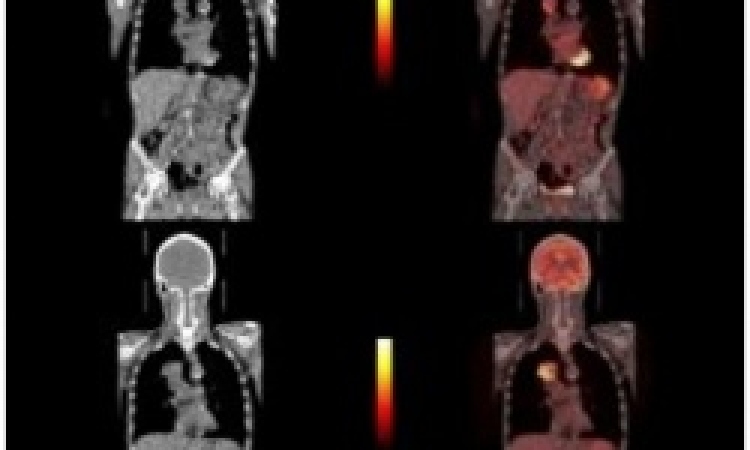
Before and two weeks after surgery, standing long-leg anteroposterior roentgenograms were taken of all patients to control for correct alignment. The mechanical leg axis was measured on these X-ray films and directly compared to the preoperative plan.
Data were statistically analysed by using a two-tailed Student’s t-test. Statistical significance was assumed at a p-value smaller than 0.01.
We can foresee that surgical robots and navigational systems will be combined in the future. This approach would use the full potential of both computer-assisted systems.
Contact: wsiebert@okkassel.de
30.04.2003