Positive action in the war against MRSA
Report: Rostislav Kuklik
The first strain of methicillin resistant Staphylococcus Aureus (MRSA) was isolated in the 1960s, and its presence was reported worldwide in the late 1990s. A higher incidence of MRSA was noted in communities, at the dawn of the new millennium, leading to two basic MRSA strains being differentiated - CA-MRSA (community acquired MRSA) and HA-MRSA (healthcare associated MRSA). In clinical practice their difference is vaguely defined; in most cases, HA-MRSA possesses higher genetic potential to express gene coding ATB-resistant protein, hence the only reliable evidence is sophisticated genetic testing bypulsed field gel electrophoresis (PGFE) for example.
Questions remained: Where do these microbes come from, and why, for example, do MRSA infections tend to appear in certain communities? The answer: MRSA is not only resulted from a natural mutual development between humans and their environment; for the most part, MRSA came to life due to antibiotic use in agriculture.
In October 1997, the World Health Organisation (WHO) organised an international meeting to address the broad (and sometimes uncontrolled) use of antibiotics as growth stimulants in cattle. Scientific evidence was presented that clearly indicated that this use directly related to human diseases, and increasing numbers of ATB-resistant microbes. The highest risk was associated with beef cattle, poultry, and pigs. Now, a decade later, medical professionals directly witness the truth of those findings: there are at least five microbes resistant to all (or almost all) antibiotics - Mycobacterium tuberculosis, Acinetobacter baumanii, Pseudomonas aeruginosa plus vancomycin resistant S. aureus (VRSA) and vancomycin resistant entorococci (VRE).
To defend antibiotic effectiveness, there is a vital need to launch a fully multi-disciplinary approach and implement strict clinical measures, by involving expertise in infectious disease medicine, microbiology, pathology, clinical pharmacology, pharmaceutical industry and, also importantly, the public.
MRSA – global threat
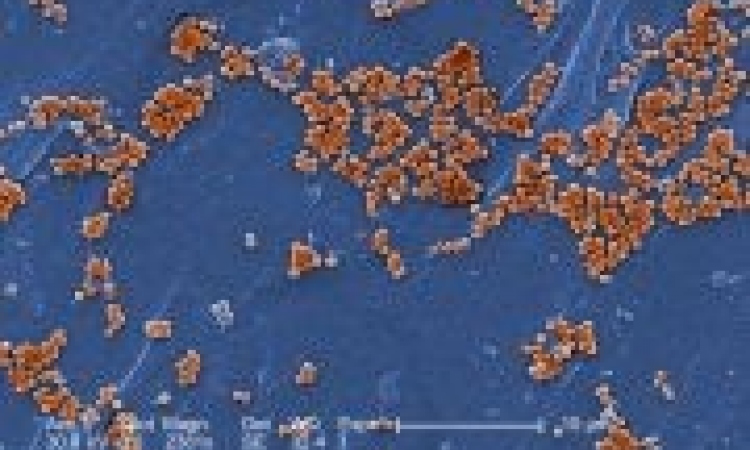
S. aureus is a gram-positive bacterium harmlessly colonising the skin of about a third of the healthy population. However, under certain circumstances it can acquire resistance to methicillin and all other beta-lactam antibiotics by expressing the exogenous mecA gene which, after translation, gives off variant penicillin binding protein PBP2’ (PBP2a) with low affinity to beta-lactams. This protein allows S. aureus to ignore ATB treatment by preventing the drug induced inhibition of cell wall synthesis.
Resistance acquired through mecA gene expression is influenced by various genetic factors, hence the level of methicillin resistance (defined by its minimum inhibitory concentration, MIC) may range from phenotypically susceptible to highly ATB resistant microbe variants.
On a global scale, MRSA strains are the most important pathogens involved with antibiotic-resistant and healthcare associated infections (their onset is typically linked with hospitalisation or intramural procedures, e.g. wound-dressing, surgery, etc.). As said, the threat is global; however, European data point to interesting facts. First, HA-MRSA strains are more frequently isolated from in-patients requiring intensive care, e.g., among the most heavily MRSA afflicted regions are Croatia, Greece, Israel, Malta, Portugal, and Turkey, where the proportion of MRSA found in intensive care unit (ICU) patients was over 60%. Second, regional differences (in both ICU and non-ICU patients) fill in a wide incidence spectrum, e.g., Scandinavia, Benelux, and Greenland reported under 5% MRSA infections, whilst the United Kingdom, France, Spain, Portugal, Italy, Croatia, Romania and Turkey reported a 25-50% incidence (as of 2007). The situation is even worse in Japan, for example, where MRSA strains are present in over 70% of all S. aureus invasive infections.
Losing the battle, winning
the war
There are basically two ways how to fight MRSA with regard to the most recent guidelines and recommendations released by authorities and key opinion leaders. No surprise these don’t differ much from what is generally recommended for successful treatment of any other infectious disease, although much emphasis is being put onto prevention, patient awareness, and utmost hygiene standard. Preventive arrangements, once the invasive infection is confirmed, must be closely followed by all involved.
Patient isolation
• Patient isolation in a specialised unit
• The attending physician must provide the patient and family with all relevant MRSA information and prevention, and advise the concerned hospital personnel
• Patient movement, e.g. to another hospital department, must be minimised
• Identification of hospital staff (as few as possible) to be in contact with the patient
Manipulation and staff precautions
• Individualise medical equipment, drugs, etc. (rule: ‘one item just for one patient’)
• Use only thoroughly disinfected equipment, disposable wrappings, garments, gloves, etc.
• Use antiseptics and skin disinfectants assiduously
• All documentation must be as detailed as possible
Patient discharge
• Document the patient infection profile thoroughly in all medical records
• Thoroughly decontaminate the patient’s ward, or room, and equipment and aids used, etc.
• Leave that hospital room unoccupied for at least 24 hours after decontamination
• Perform bacterial control sampling
Preventive measures
• Rational ATB therapy: particularly avoid cephalosporines, macrolides, and chinolones — all ATBs with the highest selection potential for MRSA (use only in clearly indicated cases)
• High hygiene standards - skin disinfectants always, face-garments (patient’s and staff) in case of patient’s upper airways infection, etc.
• Active microbiology surveillance
The above provides guidance for passive defence against microbial spread. The active method lies in reasonable ATB therapy. The following antibiotic compounds are available.
Glycopeptides:
• Vancomycin (Edicin) – 500mg i.v. every 6 hours
• Teicoplanin (Targocid) – 3x 400mg i.v. every 12 hours
Others:
• Linezolide (Zyvoxid) – 600mg i.v. every 12 hours
• Streptogramines A, B (quinupristin-dalfopristin, Synercid) – 7.5mg/kg i.v. every 8 hours
• Daptomycin (Cubicin) – 4mg or 6mg/kg i.v. every 24 hours (dosing depends on whether S. aureus bacteriemia is present or not)
• Trimethoprimum/sulfamethoxazolum (Biseptol) – 960mg i.v. every 12 hours
Conclusion – MRSA infections can be treated relatively successfully, which is very positive. However, much more emphasis should be laid on prevention and reasonable ATB prescription rather than treatment itself. ATB overconsumption and inappropriate usage helped a lot S. aureus and other bacilli to turn into the ‘superbugs’ faced in clinical settings today.
Sources: The European Antimicrobial Resistance Surveillance System (EARSS, www.rivm.nl/earss/). The Alliance for the Prudent Use of Antibiotics (APUA, www.tufts.edu/med/apua/)
01.07.2009