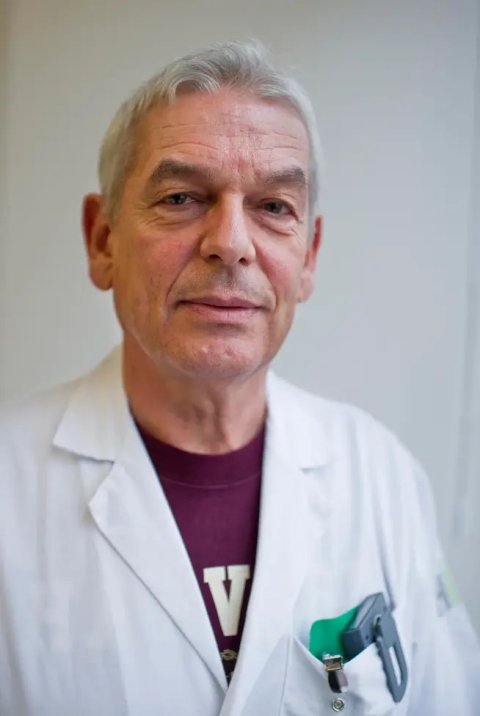
Image source: Dr Osterwalder
Article • Point-of-care ultrasound in trauma
Returning e-FAST ‘to its roots’
Stagnation, under-use, unfulfilled potential: At the EUSEM congress in Barcelona, leading emergency physician Dr Joseph Osterwalder describes how e-FAST (Extended Focused Assessment with Sonography for Trauma) – a key point-of-care ultrasound technique for trauma – has changed over the last two decades, and not necessarily for the better.
Report: Mark Nicholls
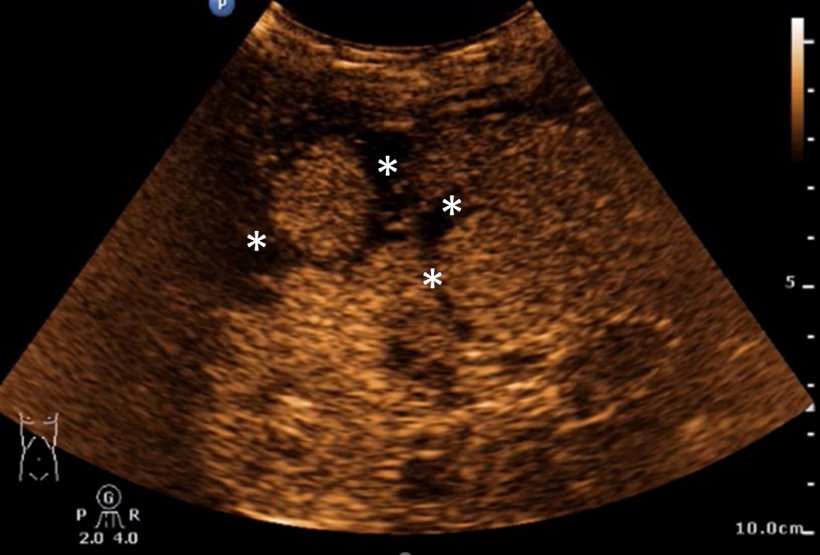
Despite ultrasound having made great progress in terms of technology, price and indications, e-FAST – a standardized protocol-based POCUS that looks for bleeding in the chest and abdomen and pneumothorax – has seen a marked, the expert added. Originally intended for the primary survey in the ATLS (advanced trauma life support) system, it is now being used for wider applications and lesser conditions.
At the European Emergency Medicines Congress in Barcelona (EUSEM 2023) in September, Osterwalder outlined how he believes that e-FAST should ‘return to its roots’ to re-define its place in imaging. ‘The traditional use was intended for unstable or non-stabilizable patients to detect large haemorrhages in the peritoneal, pleural and pericardial cavities as well as a large pneumothorax within a maximum of 1 to 2 minutes using ultrasound,’ said Osterwalder, who, until 2017, was Head of the Emergency Department at Kantonsspital St Gallen in Switzerland.
Use cases in the shock room
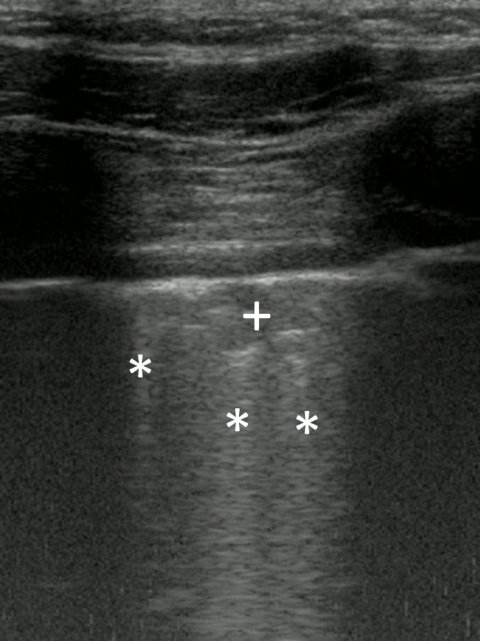
Image source: Dr Osterwalder
In stable patients, he said e-FAST should be used to detect small bleedings in the peritoneal cavity by means of four additional sonographic views; include the examination for retroperitoneal bleeding/hematoma; injuries to the spleen, liver and kidney; and free intraperitoneal air in the patient with repeat examination as necessary in the shock room. It was also intended to apply the long-established ultrasound indications during the emergency ‘ABCDE’ protocols in e-FAST patients: to look for airway obstruction, false intubation, pulmonary contusion, intracranial hypertension, retro-orbital haematoma, and fractures, and assist in monitoring and volume management.
Osterwalder continued: ‘Because musculoskeletal injuries are the most common injuries in moderate and severe trauma patients, MSK ultrasound should also be used as part of the secondary survey, especially as its diagnostic accuracy is often equal to MRI.’
Exaggerated expectations
Since the 1990s, e-FAST has been extended to stable patients and those with mild to moderate trauma, the expert said. However, he believes that this has led to exaggerated expectations, with users not fully aware of the limitations of the technique, and even resulted in studies questioning the usefulness of e-FAST.
Osterwalder points to the clear benefits for clinicians from e-FAST: more certainty for decision-making on further procedures such as an indication for CT, operating theatre, interventional radiology, and hospital admission for monitoring. ‘It also enables faster processes,’ he added. ‘There are no waiting times for CT examinations. It saves resources for teams that care for and monitor the patient, makes the attending physician more independent and also increases the degree of satisfaction.’
Patient benefit
It can improve the diagnosis and treatment of moderate and minor injuries in places with limited resources, especially CT scanners
Joseph Osterwalder
Benefits for patients include reduced risks from CT examinations such as radiation exposure, allergic reactions, and renal insufficiency from the contrast medium. The technique also avoids the need for emergency intubation in children and restless patients before a CT scan can be performed.
‘There is no evidence to date that this reduces mortality and morbidity, nor that CT leads to better results,’ explained Osterwalder, who remains convinced that redefining e-FAST has opportunities to advance the field. ‘It can improve the diagnosis and treatment of moderate and minor injuries in places with limited resources, especially CT scanners, and lead to faster assessment and care of patients in highly specialized institutions.’ He also feels there is an opportunity for industry to work more closely with clinicians.
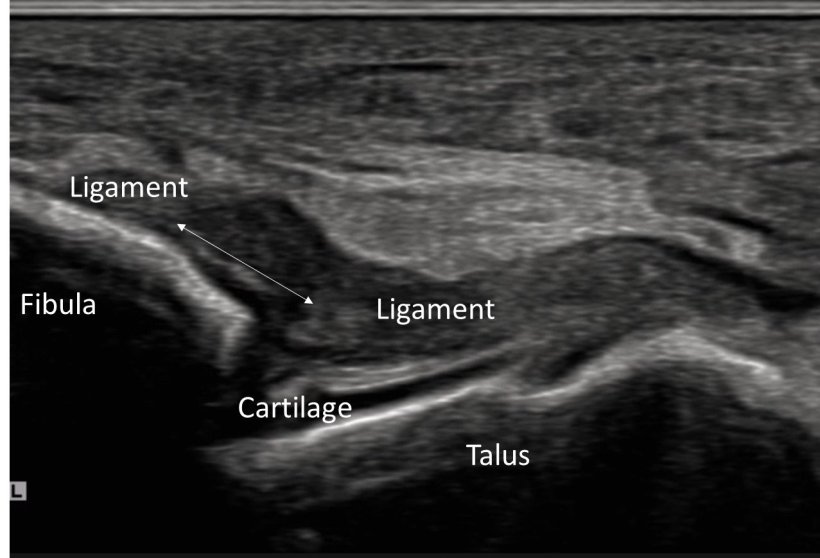
Image source: Dr Osterwalder
Wide range of applications
Osterwalder, who has significant experience operating as a field medic, further pointed out the potential of e-FAST in disaster, expedition, and military medicine. The technique is already being used in all emergency situations, not only in EDs but also pre-hospital, in the offices of general practitioners, hospital wards, ICUs, ships, expeditions, and theatres of war, he said. Application ranges from trauma, unclear shock, women of childbearing age to abdominal pain during and after resuscitation.
However, he said: ‘e-FAST has not developed any further for over 20 years, even though ultrasound has made huge progress in this time regarding technical innovations such as Microflow, better and high-resolution probes, CEUS; falling prices, hand-held devices and countless new, scientifically well-founded indications.’ He hopes that the profile of e-FAST can be raised and re-defined to ensure it is used for optimal medical and clinical benefit.
Profile:
Emergency physician Dr Joseph Osterwalder was Head of the Emergency Department at Kantonsspital St Gallen in Switzerland (1988-2017) and Associate Professor for Emergency Medicine at the University of Geneva. A former delegate of the International Committee of the Red Cross, he is a Fellow of the Swiss Society of Rescue and Emergency Medicine, the European Society of Emergency Medicine, the Swiss and German Society of Ultrasound in Medicine and is a pioneer of emergency medicine and emergency ultrasound in Switzerland.
28.02.2024





