Papworth Hospital: A constant continuing success
Recent events have again underlined the reason why Papworth Hospital in ambridgeshire, England, maintains a enowned international reputation for cardiac and thoracic procedures. As Britains largest specialist cardiothoracic hospitals, over 2,000 major heart operations were performed there in 2010. In the year ending 1 April 2011, 824
patients had coronary bypass operations, including urgent, emergency, salvage and repeat operations. Brenda Marsh reports

Mortality for his year was 0.85%, the lowest the hospital has ever achieved. Commenting on the reported survival rates for coronary bypass surgery – better than 99% for first time in the hospital’s history, consultant cardiac surgeon Sam Nashef commented: ‘These are excellent results indeed, but we are not complacent and will continue to strive for even better outcomes.’
Papworth Hospital’s clinicians have taken innovative steps in heart and lung transplantation since carrying out the UK’s first successful heart transplant in 1979, and also used mechanical devices to support patients with end-stage heart failure since the 1980s. In June, at the national Medical Futures Awards Ceremony in London, consultant cardiac surgeons Sam Nashef and Stephen Large received the Overall Winner prize in the Cardiovascular Awards and first prize in the Best Innovative Concept in the Cardiovascular Innovation category for their Temporary Cardiac Assist (TCA) device. This aims to support the heart immediately after heart surgery. Connected to the bypass machine, the device works in a similar way to an aortic balloon pump but offers significant additional advantages:
• It is immediately available after surgery as the patient is already connected to the bypass machine.
• It is far cheaper per use than aortic balloon pumps, which cost around £1,500 each.
• Potentially, the TCA can reduce the amount of time patients spend in critical care.
The TCA allows the heartlung machine, which is already connected to the patient, to operate in a similar manner to the balloon pump. It can provide immediate help at a crucial moment without the need for additional equipment, intervention and the risks and complications of using and placing the balloon pump. Mr Nashef confirmed that, because sometimes patients’ hearts need a small amount of support, often for as little as 30 minutes after heart surgery, the device provides instant access to that support – and at a far reduced cost to the NHS. ‘We are very excited to have achieved national recognition for Temporary Cardiac Assist which reflects the commitment of clinicians at Papworth Hospital to improve the quality of patient care,’ he added. ‘These awards give us an excellent platform from which to seek development funding.’*
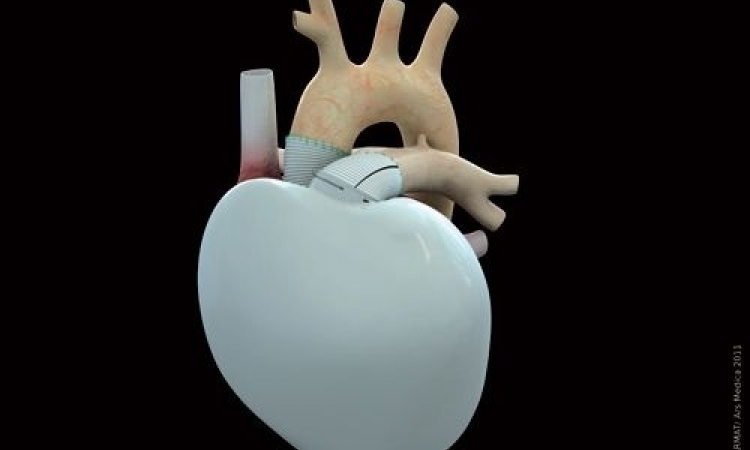
Papworth Hospital is also the only centre in the UK currently certified to implant the Total Artificial Heart (TAH) developed by the Arizona-based firm Syncardia. This modern version of the Jarvik-7 Artificial Heart designed by Robert Jarvik in the very early 1980s, is a bridge-totransplant device that received FDA, Health Canada and CE approvals in 2004 and 2005. The TAH is reported to be the only device that eliminates the symptoms and source of end-stage biventricular failure. Similar to a heart transplant, the TAH replaces both failing heart ventricles and the four native heart valves. It is the world’s first and Total Artificial Heart, and more than 900 implants have accounted for over 210 patient years of life on the device.
The TAH pumps up to 9.5 L/min through both ventricles, a high volume of safe blood flow that helps vital organs recover faster, thus helping to make patients better transplant candidates for a transplant. The partial fill/full eject design allows the patient’s body to determine blood flow based on activity level. In almost 30 years of use, the diaphragm failure rate has been less than 1% over 900 implantations. There are no motors or electronics within the body because all electronics are located outside it, in the pneumatic driver that powers the TAH and monitors blood flow. Weight: 160 grams Stroke volume: 70 ml.
Following six-hour surgery in June, at the beginning of August the first of the UK’s end-stage biventricular heart failure patients to go home with his heart replaced with an implanted plastic Total Artificial Heart left Papworth with his son and his wife carrying the Freedom portable driver that powers his TAF. This is the world’s first wearable portable driver designed to power SynCardia’s Total Artificial Heart both inside and outside the hospital. Weighing 13.5 pounds, it is designed to be worn by the patient in the Freedom Backpack or Shoulder Bag.
The transplant team at Papworth Hospital, was led by surgeon Steven Tsui, Consultant Cardiothoracic surgeon and
Director of the Transplant Service. Papworth’s transplant team had received rigorous training in Paris and was assisted by Dr Latif Arusoglu, an expert TAF surgeon from Bad Oeynhausen, Germany. The patient, 40-year-old Matthew Green, suffered Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) and his health had declined to a point where his only option was having a heart transplant.
‘We discussed with him the possibility of receiving this device, because without it he may not have survived the wait until a suitable donor heart could be found for him,’ Steven Tsui explained, adding that his patient would now be able to do a lot more than before the operation with a vastly improved quality of life ‘until we can find a suitable donor heart for him to have a heart transplant’. The Papworth Hospital Board of Directors is planning for a new 300-bed (100% single rooms) purpose-built hospital and research and education institute, all located on an eight acre site in the Cambridge Biomedical Campus.
The construction phase is expected to be complete by late 2015.
* Health Enterprise East, the National Health Service Innovation Hub for the East of England, helped with the development by supporting a patent for the device and funding prototypes for the inventors.
26.08.2011