Image source: Shutterstock/Lightspring
Article • Infection control in hospitals
Nosocomial influenza: The enormous effect of mask wearing
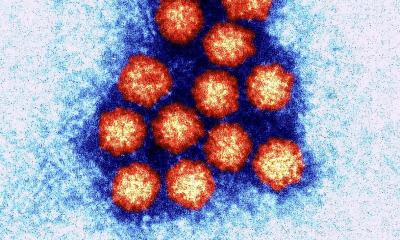
The Coronavirus dominates everyday conversation as well as medical and scientific discussions, but in a Leipzig hygiene congress, other topics – such as nosocomial influenza – took a strong position.
Report: Katrin Schreiter
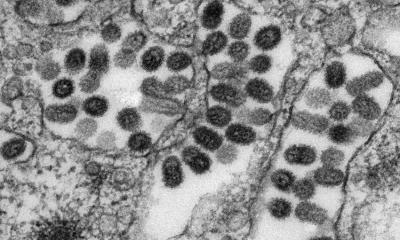
Dr Andreas Ambrosch, head of the Institute of Laboratory Medicine, Microbiology and Hospital Hygiene at the Brothers of Mercy Hospital in Regensburg, Germany, presented a new study on the spread of nosocomial influenza. But the question arises, whether this, in view of the new coronavirus, is this only an incidental topic. ‘Not at all,’ the hygiene expert exclaimed: ‘Nobody knows whether the coronavirus will still be around next year. But we are confronted with influenza every year. At the moment, everyone seems to forget how many deaths are caused by viral influenza each year.’ Reason enough for him to study the influenza virus intensively. He presented his current findings at the 6th Joint Congress of the German Society of Hygiene and Microbiology and the Association for General and Applied Microbiology, held in Leipzig.
Cancer patients are affected the most

‘When influenza occurs in a hospital, it’s particularly dangerous,’ Ambrosch stressed. ‘Up to 50% of influenza patients may die due to their underlying diseases.’ Patients on oncology wards are particularly affected, as they usually have no immunity. By comparison, the mortality rate across the total population per season is less than 0.5%.
The expert uses these numbers to confirm that prevention can indeed save lives: Ambrosch has been working on a study about the spread of the influenza virus at the 1,000 bed Hospital of the Brothers of Mercy in Regensburg since 2015. As a result, since 2017, as soon as more than three influenza patients are on a ward, all staff members have had to wear mouth and nose protection during their entire shift. The objective was to lower the high nosocomial infection rate for influenza known at the hospital and other German hospitals by 20-30%. ‘Eight hours – it sounds more dramatic than it is. But the protection is not really much of a hindrance during work,’ the doctor confirms. ‘The effect is enormous!’ he adds, pointing out the numbers.
The hospital in Regensburg sees an average of 150-380 influenza patients annually. The relatively small change of wearing protective clothing has helped to lower the rate of new nosocomial infection by 60% (from more than 20% to just under 10%), Ambrosch reports. The number of mortalities has even decreased by 85%. In 2015 and 2016 respectively, there were seven nosocomial influenza victims in the hospital; afterwards there was a maximum of only one patient a year. Consistent mouth and nose protection are also decisive in the fight against the coronavirus.
Hand disinfection is always important
Vaccination should be mandatory for medical staff. This would be a really big step in the right direction
Andreas Ambrosch
‘Obviously there are other important measures to contain, or respectively prevent, influenza,’ Ambrosch adds. ‘Hand disinfection is always important.’ His hospital has been a member of the ASH – Action on Clean Hands – for six years and has been awarded the gold certificate. But, hand disinfection alone has proven not to be enough. ‘Vaccination is the most effective measure,’ Ambrosch is convinced. ‘However, there are many shortcomings here, as the German OkaPII Study (online survey on influenza vaccination amongst hospital staff) has shown. The last nationwide survey was carried out in spring 2019, when 171 hospitals with around 27,000 staff participated. Result: only 76% of doctors have themselves vaccinated against influenza, and only 46% of nurses do. ‘To ensure effective protection more than 85% of hospital staff need to be vaccinated.’
Willingness to be vaccinated at The Hospital of the Brothers of Mercy in Regensburg also leaves a lot to be desired: ‘Only 57% of doctors are vaccinated, and only 34% of nurses. ‘We are banking on education – but only make very small steps forward.’ Ambrosch’s biggest wish regarding influenza: ‘Vaccination should be mandatory for medical staff. This would be a really big step in the right direction.’
Profile:
Dr Andreas Ambrosch is head of the Institute of Laboratory Medicine, Microbiology and Hospital Hygiene at The Hospital of the Brothers of Mercy in Regensburg, Germany. A microbiologist and Antibiotic Stewardship (ABS) expert, Dr Ambrosch has been working on an effective action plan for the protection of patients against so-called nosocomial infections – i.e. infections which patients acquire in the hospital – for the last four years.
23.04.2020