Non-invasive monitoring of airway inflammation in asthma and COPD
By Paolo Montuschi MD, of the Department of Pharmacology, Faculty of Medicine, Catholic University of the Sacred Heart, Rome, Italy.

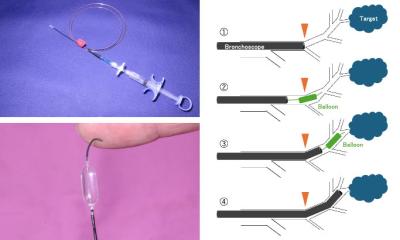
The pathophysiological role of inflammation in lung diseases including asthma and chronic obstructive pulmonary disease (COPD) is well established. Quantifying lung inflammation is relevant for the management of inflammatory airway diseases as it may indicate that pharmacological intervention is required before symptom onset and reduction in lung function. Moreover, monitoring of airway inflammation might be useful in the follow-up of patients with asthma and COPD, and for guiding pharmacological therapy. Quantification of pulmonary inflammation is currently based on invasive methods including the analysis of broncho-alveolar lavage (BAL) fluid, bronchoscopy, and bronchial biopsies, semi-invasive methods such as sputum induction, and the measurement of inflammatory biomarkers in plasma and urine, which are likely to reflect systemic rather than lung inflammation.
Interest in the identification
of non-invasive biomarkers for inflammatory airway diseases has been growing. These biomarkers should identify those patients who are more susceptible to the disease; reflect the degree of pulmonary inflammation and the disease severity; be reproducible in stable clinical conditions; be suitable for repeated measurements in the longitudinal follow-up of the patients; be elevated during exacerbations; be useful for monitoring pharmacological therapy; and be of prognostic value.
Exhaled breath consists of a gaseous phase that contains volatile compounds (e.g., nitric oxide, carbon monoxide, and hydrocarbons) and a liquid phase, termed exhaled breath condensate (EBC) that contains aerosol particles in which several non-volatile compounds have been identified. Measurement of exhaled nitric oxide (NO) is a well accepted, standardised, validated and widely used method for assessing airway inflammation in patients with asthma who are not being treated with inhaled glucocorticoids. Measurement of exhaled NO is rapid, reproducible, and provides immediate results. Concentrations of exhaled NO in patients with asthma correlate with sputum eosinophil cell counts and airway hyper-responsiveness before glucocorticosteroids. One portable analyser is commercially available and can be used to assess and monitor airway inflammation in patients with asthma on field.
Sputum induction is a semi-invasive method for assessing airway inflammation. This technique has been standardised. Sputum analysis for evaluation of percentage of sputum eosinophils directly measures airway inflammation, and is one method of objectively monitoring asthma. However, although generally considered safe, sputum induction with hypertonic saline solution can cause bronchoconstriction, particularly in patients with airway hyper-responsiveness; can induce airway inflammation by itself; can be difficult to perform, particularly in children and in patients with severe asthma or COPD; requires dedicated staff and equipment and processing of samples within two hours from collection.
Recently, attention has focused on EBC as a non-invasive method for studying the composition of airway lining fluid. Using urea, which is a freely diffusible molecule, as a marker, it has been demonstrated that a measurable fraction (1 in 24 parts) of the EBC in healthy subjects is derived from aerosolised airway lining fluid. EBC analysis of inflammatory biomarkers is a non-invasive method that has the potential to be useful for monitoring airway inflammation in patients with respiratory diseases, including children. As it is completely non-invasive, EBC also is suitable for longitudinal studies and to monitor the response to pharmacological therapy. Furthermore, different biomarkers might reflect the different aspects of lung inflammation or oxidative stress, which is an important component of inflammation. Identification of selective profiles of biomolecules in different inflammatory airway diseases might be relevant for differential diagnosis in respiratory medicine. Collection of EBC samples is simple, not expensive, and safe. However, unlike exhaled NO measurement, EBC technique does not provide real-time results as EBC samples need to be assayed for different biomolecules. Several methodological issues, including standardisation of EBC technique and validation of analytical methods, need to be addressed before this approach can be considered for applications in the clinical setting.
This article discusses the advantages and the limitations of measurement of exhaled NO, analysis of sputum eosinophils, and analysis of EBC in patients with asthma and COPD, and provides suggestions for further research in this area.
Measurement of exhaled nitric oxide
In some centres, measurement of exhaled NO is now available as a routine test for asthmatic patients. This method is useful in the diagnosis of asthma, can be used to monitor the response to inhaled glucocorticoids in patients with asthma; can predict asthma exacerbation and can be used to monitor compliance. Exhaled NO concentrations in patients with asthma decrease rapidly after anti-inflammatory therapy and are elevated during exacerbations. With the use of exhaled NO measurements, maintenance doses of inhaled corticosteroids may be significantly reduced without compromising asthma control.
Data on the concentrations of exhaled NO in patients with COPD are controversial. One important limitation of measurement of exhaled NO in these patients is that exhaled NO is strongly affected by NO content in cigarette smoke and most of the patients with COPD have a smoking history.
The clinical utility of exhaled NO measurement is currently limited to patients with asthma, as its role in the management of other respiratory diseases, including COPD, is not yet defined.
Analysis of eosinophils in sputum induction
Tailored asthma interventions based on sputum eosinophils can reduce the frequency and severity of asthma exacerbations in adults with asthma. For this reason, sputum eosinophil analysis has been proposed to adjust and monitor asthma therapy for adults with frequent exacerbations and severe asthma. The utility of adjusting asthma therapy based on sputum eosinophils compared with traditional methods (primarily clinical symptoms and spirometry/peak flow) in children with asthma needs to be established.
Although neutrophils and macrophages are generally considered to play the major pathophysiological role in COPD, up to 40% of patients with COPD have sputum eosinophilia. Analysis of sputum induction might be useful for identifying phenotypes of COPD patients. These patients are generally relatively resistant to glucocorticosteroids. However, improvement in lung function and symptoms concomitant with a reduction in sputum eosinophil counts are observed in patients with COPD with high baseline sputum eosinophilia, after treatment with inhaled or oral glucocorticosteroids. The response to glucocorticoids in this subgroup of COPD patients does not seem to be solely due to an asthmatic component, as sputum eosinophilia is not necessarily correlated with reversibility to bronchodilators and the latter is not associated with steroid responsiveness. However, the role of sputum induction in patients with COPD has yet to be established.
Exhaled breath condensate analysis
Several biomolecules have been identified in EBC and found elevated in patients with asthma and/or COPD including hydro-gen peroxide, 8-isoprostane, leukotrienes (LTs), prostaglandins (PGs), nitrites, nitrates, and nitrosothiols. In most of the studies, biomolecules in EBC have been measured with commercially available immunoassay kit, which require validation with reference analytical techniques. The presence of 8-isoprostane, LTB4, PGE2, glutathione, and aldehydes in EBC has been demonstrated by mass spectrometry analysis. pH values in EBC are reduced in patients with acute asthma and stable COPD.
Measurement of pH in EBC is easy, rapid, and provides immediate results. However, some variables including the effect of ambient CO2 and oral bacteria need to be considered. Most of the studies on EBC are cross-sectional. There are relatively few interventional studies aiming at measuring biomolecules in EBC and they are all single centre studies. The lack of standardised procedures and validation of analytical techniques is currently the main limitation of EBC analysis. Guidelines for measurement of biomolecules in EBC are available, but their usefulness is limited by the fact that many methodological issues still need to be formally addressed. Moreover, each biomarker in EBC needs to be considered separately and this makes it the standardisation of this technique more complex. However, considering the relative lack of non-invasive methods for monitoring airway inflammation and therapy, and the relevance of its potential applications, additional research on EBC analysis is warranted.
Conclusions
Measurement of exhaled NO should be used for assessing airway inflammation in patients with asthma, whereas its utility in patients with COPD is limited. Analysis of sputum eosinophils can be used to tailor and monitor anti-inflammatory therapy in asthmatic patients. This technique might contribute to the identification of COPD phenotypes with important therapeutic implications for patients with COPD. However, sputum induction is unlikely to become a routine technique for assessing airway inflammation. Identification of selective profiles of biomarkers in EBC and the pharmacological modulation of their concentrations in this biological fluid might have important diagnostic and therapeutic implications for patients with asthma and COPD. However, due to the current lack of standardisation, whether and when EBC analysis will be applicable to the clinical setting is difficult to predict.
As both asthma and COPD are heterogeneous diseases characterised by different phenotypes, the combination of different non-invasive and semi-invasive techniques, including measurement of exhaled NO, sputum induction, analysis of EBC, and possibly, new techniques using biosensors for measuring biomarkers in the exhaled breath, could be the best approach for assessing airway inflammation in the individual patient with asthma or COPD. For its important diagnostic and therapeutic implications, this approach might ultimately lead to a better management of patients with asthma and COPD.
31.08.2007