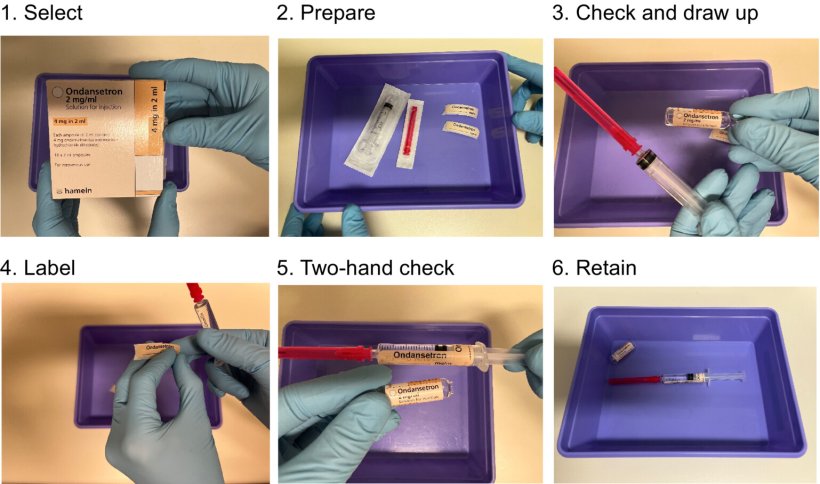
Image source: Kinsella et al., Anaesthesia 2023 (CC BY-NC-ND 4.0)
News • Safe practice
New guidance to prevent injection errors in anaesthesia
New guidance provides clear advice to reduce avoidable errors on all steps of the pathway involving injectable medications used routinely in anaesthesia care.
The guidance, which was now published in Anaesthesia (the journal of the Association of Anaesthetists), has been written by a working party of UK anaesthesia experts that include Dr Mike Kinsella, Honorary Consultant, Department of Anaesthesia, University Hospitals Bristol and Weston, Bristol, UK and Chair of the Working Party.
The authors explain: “Peri-operative medication safety is complex. Avoidance of medication errors is both system- and practitioner-based, and many departments within the hospital contribute to safe and effective systems. For the individual anaesthetist, drawing up, labelling and then the correct administration of medications are key components. These guidelines aim to provide pragmatic safety steps for the practitioner and other individuals within the operative environment, as well as short- to long-term goals for development of a collaborative approach to reducing errors. The aim is that they will be used as a basis for instilling good practice.”
This guidance has been produced by the Association of Anaesthetists in response to requests from members in view of continuing incidents of medication errors and patient harm. It ties in with the World Health Organization (WHO) 3rd Global Patient Safety Challenge 'Medication Without Harm', which was the theme of the WHO World Patient Safety Day September 2022.
Among other things, the importance, utility and enhanced safety offered by prefilled and labelled medication syringes is emphasised, as well as the use of aids such as colour-coded medication trays that can help the anaesthetist correctly organise the syringes before and during anaesthesia. Neither prefilled syringes nor these coloured aids are yet in widespread use in the UK NHS.
The authors say that labelling errors have been noted in around 1–1.25% of peri-operative medication administrations and medication substitutions in 0.2% of administrations during anaesthesia, although precise figures are lacking as research studies use different methodologies. It is important to acknowledge that every practitioner is open to error and that the risk can increase over time during a case, especially in the presence of specific factors that diminish performance such as fatigue. The authors say: “Understandably, there is considerable emphasis on medication errors. However, it is also important to give appropriate recognition to the fact that in virtually all cases the correct medication is given by the correct route, at the correct time. Good practice should be highlighted; in most cases there is a consensus on what this looks like.”
The summary recommendations of the Guidelines are as follows:
- Safe handling of medicines requires clear institutional policy within multiple departments as well as careful individual practice.
- Departments of anaesthesia should have policies for safe handling of medicines.
- Pharmacy departments should promote purchasing for safety, consistent supply and purchase from those companies complying with good labelling practice
- Prefilled syringes have multiple advantages, and their purchase and use should be promoted.
- Standardisation of fit-for-purpose physical structure and medicine storage in workplaces should be developed.
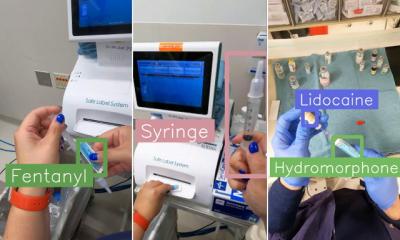
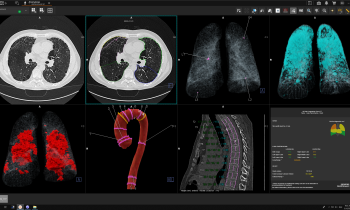
- Technological solutions that reduce the opportunity for error should be explored and adopted whenever possible.
- Standardisation of practice for syringe labelling and handling should be promoted and should form part of the curriculum for training anaesthetists. This should reduce the risk of errors when anaesthetists work together.
- Individual anaesthetists may have characteristics that affect their working; these should be recognised by the individual as well as their department, and suitable adjustments to practice made.
The authors say: “’First do no harm’ is what doctors strive for. We hope that these guidelines provide useful points for anaesthetists’ individual practice, while acknowledging that patient safety also relies on supportive systems within their hospitals.”
Source: Association of Anaesthetists of Great Britain and Ireland
10.08.2023