MRI Alert!
The scanner shortage in France is a scandal, says chairman of the French Society of Radiology. New MRIs must be installed in 250 emergency departments
The French Society of Radiology (FSR) is going public with its case that the lack of access to medical imaging equipment has reached a critical state in France and that this is threatening responsible clinical practice. Disappointed with the role radiology is given in the French governments policy and the refusal to increase MRI capacity, the FSR has drafted a 10-point Plan Imagerie.
In an interview with John Brosky, our Paris correspondent, at the society’s congress this October FRS Chairman Dr Jean-Pierre Pruvo discussed the crisis and the 10-point Plan Imagerie drafted by the society to improve imaging problems in France.
Dr Jean-Pierre Pruvo, Chairman of the French Society of Radiology, is taking his arguments that the lack of access to medical imaging equipment in France has reached a critical state and is threatening responsible clinical practice, directly to the President of the Republic, Nicolas Sarkozy. Along with setting the agenda for that discussion with the President’s mediator, Dr Pruvo has begun a lobbying campaign with the heads of the French Senate and Assembly.
‘The degradation of imaging capabilities in France, specifically for magnetic resonance imagery (MRI) has been allowed to go on for some time,’ explained Dr Pruvo. We have repeated our concern for years. Ahead of the new reform law Hospitals, Patients, Health and Regions (HPST) we were asked by the Marescaux Commission to provide our perspectives on radiology in France and were pleased to see, in the final report, that there is a recommendation to respect the model of the University Hospital Centres (CHU) at the heart of French healthcare and, further, that the Commission insisted on the necessity for a high level of quality for the imaging platforms at the CHUs. The Commission’s recommendations, if followed, would have allowed us to catch up with the shortage of medical imaging capacity in France.
‘Yet, in the final HPST law we were very disappointed by the position given to medical imaging in France. Today we have radiologists and clinicians who simply do not have access to these critical modalities of MRI or computed tomography (CT) scanners and are forced to perform examinations with ultrasound or conventional X-ray that serve no clinical purpose.
‘This is not to criticise colleagues. They do not have the equipment and are working with the tools they have, such as ultrasound and X-ray. Instead we are critical of a government that on one hand resists installing the needed MRIs and CT scanners but says nothing about reimbursing these unnecessary and often useless examinations with other modalities.
‘In 2010 we will come to the end of the current plan for funding medical equipment and in the new planning cycle for the new regional authorities created by the HPST law there is no policy to increase authorisations for MRIs. This does not make any sense. We are walking on our heads, as we say, in France.
‘We urgently need 250 MRI scanners, one for each of the emergency centres in France. Where we are behind in a serious way with MRIs is for emergency medicine. The continued policy of the government authorities is inexplicable. This has gone on for years without any response. For this reason I will be meeting with the President.
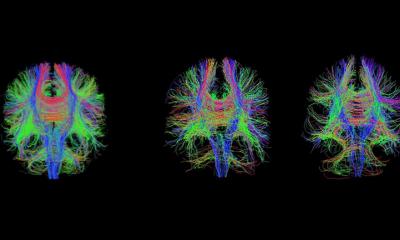
‘The CHUs in France are struggling. We are sending out an alarm with our Plan Imagerie, asking for the same priority that the Ministry of Health has given in the past with programmes such as the Cancer Plan. My approach is to argue the clinical needs and not to compare France with other European countries. I will tell the President, and the Minister of Health, that we have 2,500 incidents of strokes per million population in France, yet none are given an MRI examination on arrival at a hospital. This is a scandal! Where they are available, the patient is given a CT scan, which as a neuroradiologist I can tell you are useless for diagnosis. I will tell the President to give us 250 MRIs urgently needed need for cranial exams.
‘We have hundreds of thousands of women in France at risk for breast cancer, who have a known history of cancer in their family, yet we do not have the means to provide a breast examination by MRI, which is clinically proven to be superior for detection than conventional mammography. This is not medically responsible.
‘I will argue the business case, that we have families with a history of colorectal cancer who undergo colonoscopy with general anaesthesia when a clinically effective and cost-effective examination would be a virtual colonoscopy with a CT scanner. But we are not able to provide these screenings for these at risk patients. Virtual colonoscopies would free up operating rooms and lower costs for the healthcare system. I have 20 concrete clinical cases like this to present. Yet the bottom line, the most emblematic response, is to authorise 250 MRIs of 1.5 tesla for emergency departments across France.’
Wouldn’t such a programme be very costly? ‘No!’ exclaimed Dr Pruvo. ‘It is the opposite case. We cannot afford to continue spending on unnecessary examinations and the inefficiencies in healthcare that they create. Investing in MRI would reduce costs for France. Practice guidelines nearly always recommend a direct access to CT scanner or MRI exams. If we have these examinations, we avoid other, unnecessary examinations saving money and especially saving time in patient care.’
Plan Imagerie
‘This calls for a serious study of the costs and benefits of medical imaging for France. We suggest a reduction in the length of hospital stay, that enacting good practices will lead to the prevention of disease, that reducing waiting lists for examinations -- and the consequences of these delays for exams -- will all save on healthcare spending. There are diverse areas affected, such as the reduced costs for transporting ill patients, and then a wide area of social repercussions, which can be significant, starting with lost time at work.
For example, if you have severe sciatica, in most countries you are given an MRI exam immediately. In France you wait for weeks. You are given an X-ray, which is expensive. You are put on medication for the pain and that costs more. You are unable to work. Finally, you have your MRI scan, but this only restarts the entire diagnostic process that could have begun right away without these extra costs and delays.
At the radiology congress it was suggested the government is passive about the declining MRI situation because to purchase scanners would also require that they reimburse the costs of the medical exams performed with those scanners. ‘Even private clinics that have the funding and want to buy an MRI need to receive government authorisation to go forward -- and they are blocked. A colleague in private practice complained to me that that he needs an open MRI for obese or elderly patients, but that he was denied his request. And yet, the government does not hesitate to pay for unnecessary imaging exams.
The Plan Imagerie from the Society calls for a revision of the system for authorising equipment, specifically for MRIs and CT scanners. And another one of the 10 points in the Plan calls for re-inventing the modalities of reimbursement for radiologists in both public and private practice, permitting the two sectors truly to collaborate.
‘The Plan asks for a good medical imaging platform for each CHU with a correct balance of the modalities required and a sharing of these resources across the different medical specialties. Beyond patient care, in the area of research the number of papers published by French physicians each year has begun to diminish and this is directly related to their access to MRI. Medical imaging, and most often MRI, is at the heart of many clinical studies, and we are less and less sought out for participation in these studies. These CHUs are the centres for medical education and research in France, where young doctors conduct clinical evaluations and improve patient care. And they do not have the equipment they need. The equipment we do have is aging and it is not being replaced, not to mention the need for enhanced capabilities.
‘Finally Plan Imagerie covers the needs for radiology archiving and networks. We have a very strong point on teleradiology, connecting radiologists for expert consultations, but also to connect us so that we can stay closer to the patient care processes.’
12.11.2009