Article • Microsurgery
Lower limb trauma – reconstruction or amputation?
‘Amputation v. reconstruction’ – a vital issue – was debated by two leading surgeons during the Microsurgical Lower Limb Reconstruction session at the Advances and Controversies in Reconstructive Microsurgery (ACRM) 2016 conference, held in the United Kingdom this May. Consultant Plastic Surgeon Umraz Khan, from North Bristol NHS Trust presented a plastic surgeon’s view, while Ben Davis, a Consultant Orthopaedic Surgeon at the Norfolk & Norwich University Hospital, discussed the perspective of an orthopaedic surgeon. During our interview, Khan explained that an important question is ‘What constitutes a useful limb?’ and any decision to amputate or salvage a traumatised lower limb depends on a number of requisites being in place.
Report: Mark Nicholls
Amputation is, by definition an all or nothing event that should be reserved until it is clearly necessary.
Ben Davis
‘An important requisite is that there must be no chronic pain,’ he continued. ‘The difference with the lower limb is that it bears weight and if every time a patient puts their foot down it hurts, they will limp and that will have a detrimental effect on the more proximal joints, the hip joint or the back, for example. The patient then becomes addicted to painkillers and they are better off losing the limb. Pain is an important consideration and a reconstructed limb should be pain free.’ He also stresses that ‘reconstruction should be within the realms of possibility’ and, whilst surgery may be technically possible, if it leaves the patient with significant morbidity the solution is not to do reconstruction.
Scoring systems are available to help a surgeon to decide, although he said the clinical experience of the surgeon remained the critical factor. Advances in technology and surgical practice have changed the approach to lower limb trauma, and the prospect of limb transplantation is also on the horizon. ‘We are able to grow bone, which we could not do reliably before,’ Khan pointed out. ‘If someone had bone loss it was almost certain amputation in the past, whereas now we can grow bone in a frame and the plastic surgeon is involved in providing microsurgery for that.’ The demographic of patients is changing, shifting away from young adult males involved in road accidents towards older active early retirees.
Amputation rates are falling and, Khan explained, ‘While there are some patients who have a futile reconstruction and have a delayed amputation either through infection or pain, which used to be up to 30 percent two decades ago, but has come down to about three to four percent because we are making the right decisions about the patient – and it is the surgeon’s experience and decision making that has a massive impact for the patient in the long-term.’

Davis, who believes that salvage of a limb, or as much as circumstances allow, is the preferred option, highlighted the bespoke nature of every case. ‘There is a tendency for surgeons to assert very blunt and incorrect conclusions about the rapidity with which patients can be mobile and active after amputation, but those conclusions are generally wrong,’ he suggests. ‘Amputation is, by definition an all or nothing event that should be reserved until it is clearly necessary.’ During the ACRM session, he highlighted how the ‘decision regarding amputation and salvage of the lower limb is complex and there is no algorithm, formula or protocol that can be applied to an individual patient.’
Both surgeons acknowledge the significant development of prosthetics, however, Davis warns that while the success of the Paralympic Games and publicity surrounding the rehabilitation of military personnel highlights the amazing potential of prosthetics, the level of rehabilitation and the motivation of these individuals is not representative of the general population. ‘At the same time as prosthetics advance, so does the technology and understanding of tissue engineering and implants, creating salvage options where previously none existed,’ Davis added.

In terms of salvage, 3-D printing and tissue engineering are likely to enable the bespoke creation of mechanical and biological implants for individual problems and more reliable and sophisticated implants for limb lengthening are already available and being used with great success, he pointed out. ‘In prosthetics, the use of osseo-integration is under-going a resurgence of interest and the possibilities created with computerisation, robotics and power assistance will continue to drive forward prosthetic possibilities,’ Davis explained.
But, he warned that, when looking to amputate or salvage, the patient’s wishes and perspective are paramount in the decision-making. ‘From a patient’s perspective, having your own stable functional limb is unlikely to ever be bettered,’ he said. ‘If, however, a patient is living with a chronically painful, poorly functioning limb and has reached the end of the salvage options, or has reached the decision themselves that they no longer wish to continue with salvage, then amputation can be a very positive step forward.’
Profiles:
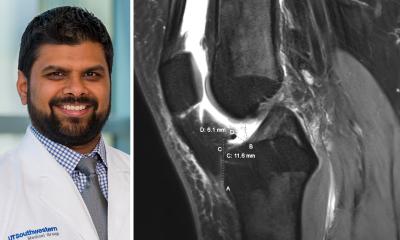
Umraz Khan is a consultant plastic surgeon at the North Bristol NHS Trust. He publishes regularly on different aspects of patient trauma with a specific area of research focused on ways of improving functional outcome.
Ben Davis is Consultant Trauma, Orthopaedic and Limb Reconstruction Surgeon at the Norfolk & Norwich University Hospital. His research interests lie in outcomes in trauma surgery, non-union, fracture healing and external fixation.
16.09.2016