Article • ESC consensus statement
Intracoronary imaging advances
Interventional cardiologists have been aware of the value of intracoronary (IC) imaging in clinical practice for more than twenty years. However, recent developments and improvements in modalities and software have enabled huge strides in its range and scope for both diagnostic assessment and in percutaneous coronary interventions.
Report: Jane McDougall
Imaging options now include intravascular ultrasound (IVUS), optical coherence tomography (OCT) and near-infrared spectroscopy. This organic growth has created significant differences in the use of IC imaging across regions and institutions.
Generally speaking, IVUS is the most established IC imaging technique, used in more than 80% of PCI cases in Japan, but OCT the equivalence of which has now been confirmed, is increasing in popularity. In an attempt to homogenise its application, the European Association of Percutaneous Cardiovascular Interventions (EAPCI) has generated frequent consensus statements on its utility, drawing on clinical evidence from imaging studies and best practice experience.
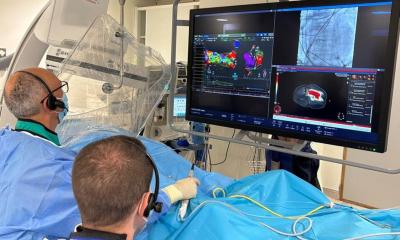
The ESC revascularisation guidelines strengthen the indications for IC imaging by recommendation. In light of these new recommendations there was an official presentation of the consensus statement at EuroPCR and also a training session presented by two of the authors; Thomas W Johnson from Bristol, United Kingdom, and Francesco Prati from Rome, Italy.
Delineating the extent of coronary artery disease
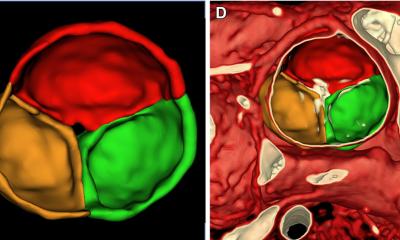
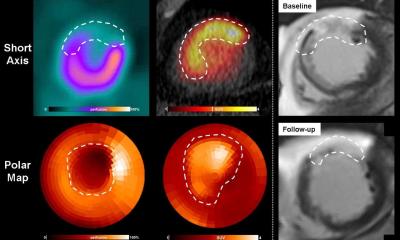
Intracoronary imaging provides an adjunct of information to angiography and, therefore, is invaluable for delineating the extent of coronary artery disease and characterising the severity of atherosclerotic lesion(s), which may appear ambiguous from angiography alone. Angiography overestimates lumen dimensions and is limited by its two-dimensional view of a three-dimensional structure which, as a consequence, results in poor and/or inaccurate estimations of plaque volume, morphology or lesion severity. All of this information can be more precisely obtained by intravascular imaging, OCT being of particular use in thrombus detection because it can distinguish between red (due to the optical attenuating properties of red blood cells) and white thrombi, the difference between which dictates the choice of pharmacological management.
The IC-imaging training session at EuroPCR considered its role in three areas:
- Defining and optimally treating calcified coronaries: coronary plaques can be classified based on the amount of calcium in a lesion. The presence of segments with partially calcified or calcified plaque has been suggested to have a significant effect on mortality; therefore, the use of intracoronary imaging to assess and guide modification strategies for high-burden calcification is increasing. Calcified plaque is brightly echo-reflective and creates a dense shadow, as well as reverberation markers that appear radially at spaced intervals from the calcified segment. With electronic callipers and computerised planimetry, accurate quantitative measurements can be made at the narrowest cross-section to determine the minimal luminal area (MLA) and diameter and at another ‘normal’ segment (within 10 mm of the culprit lesion) which is used as a reference for the healthy diameter of the vessel. This allows calculation of the percentage stenosis, plaque area and plaque burden and guides appropriate treatment strategies.
- Understanding the potential of intracoronary imaging to define the aetiology of atherosclerotic ACS and to guide management: determining lesion morphology has direct implications for the treatment strategy to be implemented. Historically, treatment in ACS has been focused on stabilising thin-cap fibroatheroma associated with thrombus formation. However, the widespread use of IC-imaging in research, particularly OCT has shown that in one-third of all ACS and one-quarter of STEACS are caused by plaques with an intact fibrous cap, the majority seen as eroded plaques. Identification of this type of plaque means treatment can be tailored to the individual characteristics of the patient’s disease. Plaque erosion, characterised by endothelial denudation, tends to occur in younger patients including pre-menopausal women and is associated with active smoking in an absence of traditional factors for heart disease. Generally, its treatment is associated with better outcomes than plaque rupture and if correctly diagnosed can be conservatively treated.
- How to delineate and manage non-atherosclerotic ACS presentations: Historically, IC-imaging has concentrated on the use of intracoronary imaging in pre-PCI assessment in patients with acute coronary syndrome (ACS). In the stable population angiographic ambiguity occurs under many circumstances, when there is excessive plaque burden, calcification, old plaque rupture, coronary tortuosity, or aberrant vessel anatomy.
Under those conditions, intracoronary imaging provides clarity, revealing the detail within the vessel. Careful acquisition of angiographic and IC imaging has created a reliable database that facilitates analysis of IC images, however, correct interpretation still requires a considerable level of expertise, training and experience.
Despite being with us for more than 20 years, intracoronary imaging is still pushing forward the boundaries of what can be achieved in interventional cardiology. Newer probes, bluetooth and Wi-Fi connections mean that imaging is an integral part of the Cath lab, used at all stages of intervention. The technology is advancing rapidly with higher resolution images, faster acquisition times, combined techniques and a mass of data that can be mined to provide all the clinical evidence required to drive the field. It is quite clear, by the array of options on display at EuroPCR, that the future of intracoronary imaging-guided PCI is very exciting.
31.08.2019