Improved specificity in breast ultrasound
Sonography is the most important non-invasive supplementary procedure to mammography, the current gold standard in breast cancer diagnostics. High-resolution ultrasound can reliably distinguish cysts and solid lesions.
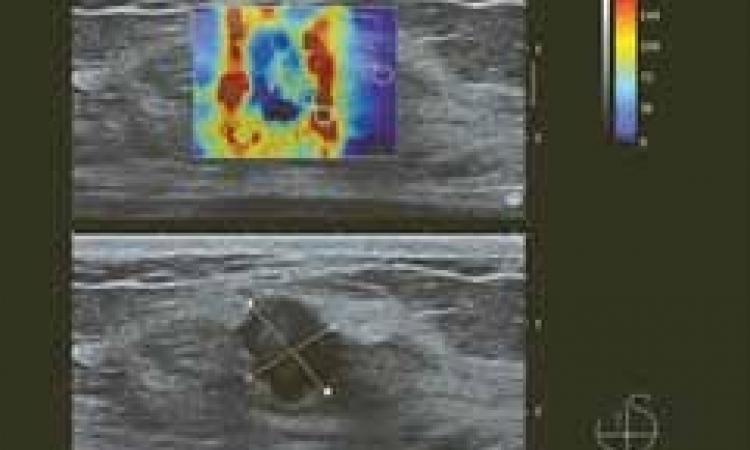
Bottom: B-mode sonography, hypoechogenic, oval, smoothly delineated mass, BI-RADS 4a, fibroadenoma was histologically confirmed.

However, efforts are being made, in clinical practice and in research alike, to develop sonographic procedures that help determine malignancy or non-malignancy of masses. The BE1 Multinational Study of 939 Masses, whose results will be presented at the Satellite Symposium of this year’s European Congress of Radiology (ECR), offers first validated data.
The authors of the study arrived at three key conclusions:
• The supplementary use of ShearWave Elastography reduces the number of superfluous biopsies in certain BI-RADS (Breast Imaging Reporting and Data System) 4a masses and allows certain masses to be downgraded to BI-RADS 3, a category in which the malignancy rate is below 2%. Under certain circumstances
ShearWave Elastography may also corroborate tumour suspicion in BI-RADS 3 masses (and involve a reclassification of the lesion to BI-RADS 4a to catch a cancer that would otherwise have been missed.)
• Certain BI-RADS 3 masses that require follow-up can, in combination with shear wave elastography be downgraded to BI-RADS 2 and can thus be followed up in the usual intervals.
• ShearWave Elastography is a valuable supplementary procedure to conventional ultrasound in breast cancer
diagnostics.
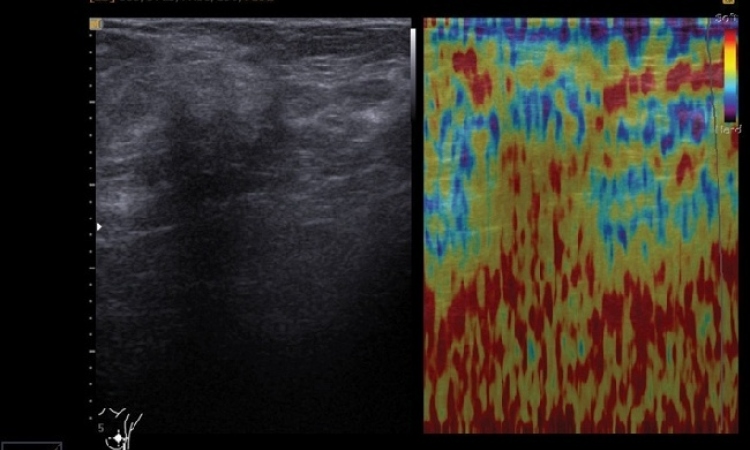
During this international study at 17 renowned US and European breast cancer centres, more than 1,800 tumours with histopathological findings were examined with ShearWave Elastography. While elastography is a very exciting development in ultrasound, ShearWave Elastography, which measures tissue elasticity with the help of shear waves, is the most recent innovation in this area.
The technology, which is based on ultra-fast imaging, is user-independent since it does not require
manual pressure. In ShearWave Elastography, shear waves are generated in the tissue and their speed
of wave propagation is measured. Thus the radiologist can assess tissue elasticity and stiffness. In 2009,
University Hospital Schleswig-Holstein (UKSH) Campus Kiel was the first hospital in Germany to introduce
ShearWave Elastography. Out of the approx. 5,000 patients examined with ShearWave Elastography so far in Kiel, 250 underwent the procedure for this study.
Fritz Schafer MD, Head of Mamma Diagnostics and Interventions at UKSH Campus Kiel, and his team, wanted to know whether it might be possible to avoid certain breast tissue biopsies in the future. While suspicious
masses continue to require additional histological assessment, for certain low-suspicious masses stressful biopsies might no longer be necessary in the future. In the present study, several models were examined to evaluate different ShearWave features. The aim was to identify the best transcriptor for a reliable diagnosis. The study indicated that particularly masses of BI-RADS categories 3 and 4a could be better assessed with ShearWave Elastography. Masses in BI-RADS category 3 have a 98% probability of nonmalignancy.
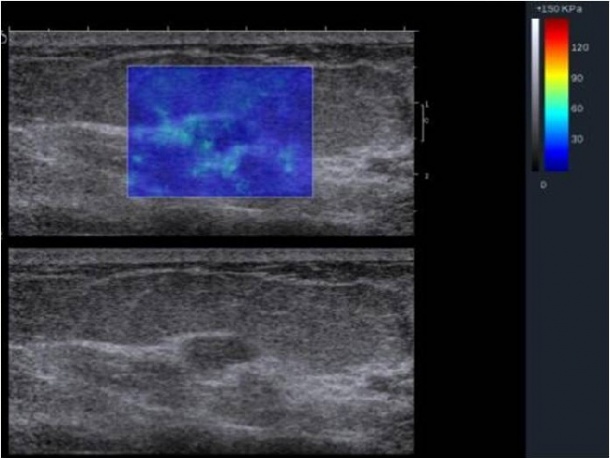
Further follow-up at six months is recommended in this category. ‘An important result of the study says that with maximum elasticity (Emax) of 160 kPa and higher, or non-homogenous findings (Ehomo) in ShearWave Elastography, the lesion should be upgraded from BI-RADS category 3 to 4 since these parameters indicate a high probability of malignancy,’ radiologist Dr Schafer explains. Masses in BI-RADS category 4 have a probability of malignancy between 3 and 94%. In this category the pertinent question is which lesions might be malignant and how these lesions could be described more precisely. Researchers looked at ShearWave Elastography for reliable indicators to downgrade masses from category 4a into category 3. ‘If Emax is 80 kPa, or less, and if the findings are rather homogenous and if high-resolution ultrasound shows solid findings with benign criteria, the mass can be downgraded from BI-RADS 4a to 3.
‘The two criteria Emax and Ehomo increase specificity by 29-34% compared to high-resolution B-mode ultrasound,’ he points out. Patients with a downgraded mass must be monitored, but a biopsy is no longer required. If the maximum tissues stiffness is 20 kPa or less, the mass might even be downgraded from BI-RADS category 3 to 2.
####
Source: Radiology: Volume 262:Number 2 – February 2012 pp.435-449, www.radiology.rsna.org
21.02.2012