Imaging and stroke
Report: Kerry Heacox, i.t. Communications
USA - Although it is well know that the speed of diagnosis and treatment for stroke victims is of paramount importance (4.5 hours), not all US hospitals have stroke expertise. The Joint Commission, the organisation responsible for accrediting US non-government hospitals, has certified only about 500 out of several thousand hospitals as primary stroke centres.
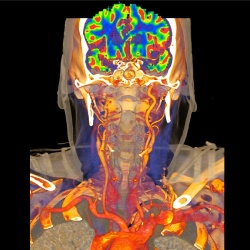
Images produced by CT, CT Angiography (CTA) and MRI scans can extend the therapeutic window of treatment, improve efficacy, and limit complications. Imaging is performed to identify the presence of haemorrhage, of an intravascular thrombus that can be treated, of irreversibly infarcted tissue and the size of its core, and/or of hypoperfused tissue at risk.
However, precisely what imaging procedures should be performed and which offer the greatest patient benefit is controversial. In fact, the International Stroke Conference included a point/counterpoint debate on whether a non-contrast head CT scan is the only imaging procedure needed within the 4.5 hour window. The appropriateness of performing delayed interventions based on diffusion-perfusion imaging was also debated.
Non-contrast CT can exclude haemorrhage, CTA can identify intracranial thrombus and vascular narrowing, and perfusion CT can differentiate between penumbra (brain tissue at risk, but viable and potentially salvageable) and irreversibly damaged brain tissue. Non-contrast CT scans are typically the first to be performed to evaluate acute ischaemic stroke because they are fast, safe, and installed in almost every hospital. Multidetector CT scans can be performed in seconds. Perfusion CT exams using non-ionic iodinated contrast are also very fast when performed with high performance CT scanners.
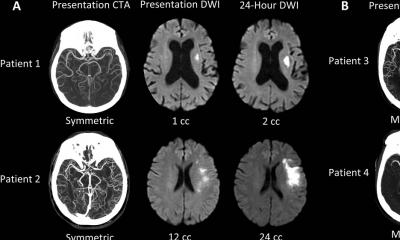
MR diffusion-weighted imaging is the most sensitive, specific technique available to identify acute infarction, and can be combined with MR perfusion to differentiate viable from nonviable tissue. MR perfusion weighted imaging enables capillary perfusion to the brain to be measured, and contrast-enhanced MR angiography is ideal for extracranial artery imaging.
Both CT and MRI technologies produce images that have similar information. A disadvantage of MRI imaging is that the exam may take more time and radiographers may need special training to work rapidly. However, MRI imaging provides direct visualisation of the full extent of infarction and provides whole brain coverage that allows physicians to identify small but clinically relevant hypoperfusion areas. High radiation dose exposure is also not an issue.
Barriers to advanced imaging
Dr Max Wintermark, one of the point/counterpoint presenters at year’s International Stroke Conference (9-11 Feb, Los Angeles) and Dr Carlos Leiva-Salanas, both neuroradiologists from the University of Virginia in Charlottesville, identify two barriers to implementing advanced imaging for stroke patients -- lack of standardisation and lack of validation, especially for perfusion/penumbral imaging.
The Stroke Imaging Repository Consortium (STIR) recommends that both commercial and academic hospital-developed perfusion/penumbral imaging software be systematically compared and harmonised so that a stroke patient scanned on any CT or MRI scanner will be diagnosed with similar values in terms of the volumes of infarct core and penumbra.
The neuroradiologists support automation and quantification as being critical for standardisation of perfusion processing. Two clinical trials, DEFUSE 2 and MR RESCUE, are using automated software to assess brain perfusion in less than five minutes.
In this age of cost-cutting, and with too many CT, CTA, and MRI types of examinations to mention, there is increasing pressure to cost-justify diagnostic imaging procedures based on patient outcome. Many clinical trials are needed to validate advanced neuro-imaging techniques. Some are underway, others await sponsors and funding.
Clinical trials are especially needed for women patients. According to American Heart Association statistics, about 55,000 more women have strokes in the USA and they represent about 60% of all stroke-related deaths. The survivors also have worse outcomes than men. In an American Journal of Roentgenology article (Feb 2011) about the role of radiology in diagnosing women with CVD, radiologist Dr Ricardo C Curry (Baptist Centre and Vascular Institute, Miami) strongly advocates the need for more research to determine if imaging can lead to early diagnosis, changes in clinical management and overall improvements in the outcomes of female stroke patients.
02.03.2011