Hyperpolarised Helium MRI of the lungs
Andrea Martini and Joerg Larsen, of the Institute for Roentgendiagnostics, Braunschweig Teaching Hospitals, Germany, present an introduction to the pulmonary ventilation and diffusion imaging by MRI
Only few imaging modalities lend themselves to imaging of the lungs. Conventional chest radiography is the most commonly used tool in the investigation of pulmonary pathology but yields the perhaps most difficult, plain radiographs to interpret.
Given the inherent density differences in lung parenchyma, computed tomography (CT) permits high contrast resolution in lung imaging, although the assessment of very peripheral airways remains limited. In contrast, scintigraphy techniques allow imaging of ventilation and perfusion, but lack spatial resolution. All of the aforementioned techniques also carry a radiation penalty. However, the possibility to combine imaging of both structure and function in a non-invasive magnetic resonance imaging (MRI) examination, as performed anywhere else in the body, is hindered by the lack of free water, which renders the lungs signal deficient on conventional proton MRI. In addition, the innumerable air-soft tissue interfaces in pulmonary parenchyma do cause considerable susceptibility artefacts.
Nonetheless, while hydrogen is the most frequently imaged nucleus in MRI, due to its great abundance in virtually all other biological tissues, any nucleus with a net nuclear spin may principally be explored by MRI. The non-radioactive noble gas isotopes 3Helium (He) and 129Xenon, for example, may be inhaled and serve as contrast media in the determination of air space distribution within the lungs. While the nuclear density of these gases in their unprocessed state is too low to produce a useful signal, polarisation techniques can increase nuclear spin polarisation by 4-5 orders of magnitude, yielding a proportionally spectacular signal on dedicated MRI examination. This allows fast breath hold imaging and holds the promise of enhanced sensitivity and contrast in pulmonary imaging, a new technique that was first experimentally explored by US researchers in guinea pigs (Middleton H et al., Magn Reson Med 1995;33:271-5).
Polarisation using so-called optical pumping methods produces spin alignments, i.e. the spins of the gas atoms, which act as small dipoles, align into one direction, causing ‘macroscopic’ magnetisation. Polarisation is transferred from polarised laser light when Helium principally absorbs the polarised light. The resulting gas may be compressed, making it storable in low gradient magnetic fields for several hours (up to six days), also allowing transporting it to remote sites for imaging applications.
MR system requirements for He-lung MR imaging (He-MRI) include a broadband radio-frequency system, such as that used in MR spectroscopy applications and dedicated receiver coils operating at the He-frequency. Owing to the decay characteristics of the polarised gas, as well as the need to consider cardiac pulsation and respiratory motion artefacts, fast low flip-angle (gradient echo) sequences (fast 3-D coronal FLASH, dynamic transverse-axial 2-D FLASH) are employed.
While Xenon has known anaesthetic properties due to its significant solubility in biological tissues, Helium is chemically inert and absorbed only in negligible quantities. No adverse effects have thus been reported with its use.
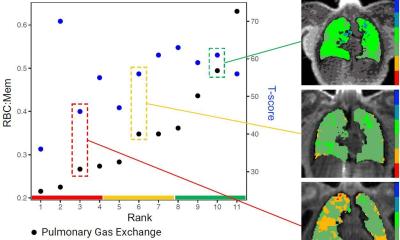
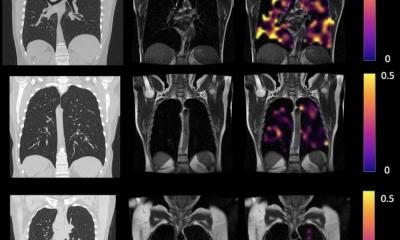
There are three particular approaches to the use of hyperpolarised helium imaging. First, pulmonary Helium content may simply be quantified, a test that is no different from a gadolinium enhanced MRI- or iodine enhanced CT-scan. The patient inhales the agent and a cross-sectional scan is performed, usually in the axial or coronal planes (see above). The distribution of Helium then equates to the pulmonary ventilation. Second, the diffusion capacity of the lungs may be measured. In a healthy lung, the branching of the bronchial tree results in a reduction in airway size towards the lung periphery. Ultimately, in the alveoli, where gas exchange takes place, diffusion capacity is limited. In contrast, in many chronic pulmonary diseases, such as emphysema, the peripheral airways are widened, resulting in a loss of restricted diffusion, which can be accurately assessed on apparent diffusion coefficient mapping. Finally, polarised Helium degrades when in contact with oxygen, with consequent loss of its MRI signal properties. This fact may be exploited, permitting an indirect measurement of oxygen concentration through repeated scanning in short intervals when signal decrease can be monitored.
Consequently, clinical applications for these techniques are plentiful. Being able to consider the homogeneity of ventilation is priceless in the investigation and management of patients with COPD, asthma as well as cystic fibrosis and other paediatric chronic lung disease in particular. Asthma and COPD are the commonest airway diseases and associated with considerable morbidity and mortality. The desire to consider their progression has long been hampered by the lack of sensitivity of current techniques and further impeded by the need to use ionising radiation. More frequent follow-up examinations, now possible through the introduction of He-MRI, may become integral to the evaluation of new treatment regimes, also permitting post-treatment examinations, even in the very short term e.g. after physiotherapy. The methods may also be useful before and after lung transplantation and in the evaluation prior to volume reducing lung surgery. However, such MRI examinations require patient compliance, consequently making them more difficult to undertake in babies and small children.
In this context, two seminal studies have provided crucial evidence of the worth of MRI using noble gases as contrast agents: Salerno and co-workers could demonstrate that He-MRI correlates with spirometric indexes in patients with established emphysema (Radiology 2001;222:252-60), while Fain et al. have since shown that He-MRI may even detect early emphysematous changes in asymptomatic smokers (Radiology 2006;239:875-83).
Clinical pulmonary function tests provide overall information on lung function, i.e. they consider both lungs together. Current lung imaging suffers limited spatial resolution and carries a radiation penalty. Hyperpolarised Helium MRI is an emerging technique that may overcome these difficulties, a notion that is reflected by a rise in scientific publications on this subject in recent years. However, hyperpolarised gases are not commercially available and produced by only a few centres worldwide. The logistics of production and delivery to imaging sites, together with the costs of agents, therefore limit the general usefulness of the technique for the foreseeable future (Kauczor HU, Br J Radiol 1998;71:701-3). Nonetheless, when these difficulties can be overcome such as recently at Sheffield’s Children’s Hospital (UK), very considerable benefits are to be gained, specifically for patients with chronic lung disease.
A referenced version of this article is available upon request by contacting J Larsen MD FRCR, Consultant Radiologist, at j.larsen@klinikum-braunschweig.de.
30.04.2008