Hopes for new treatment
Researchers have discovered a potential new treatment for diabetes by isolating and killing defective cells which prevent the natural production of insulin. The investigation opens the door to a potential therapy for patients with type 1 diabetes.
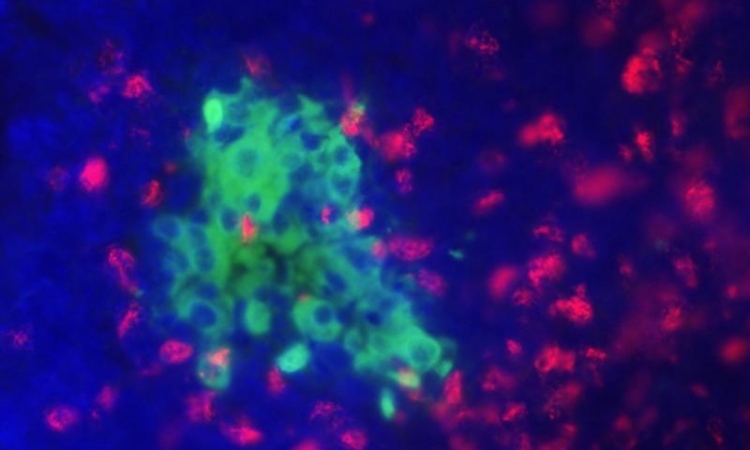
Type 1 diabetes is an autoimmune disease in which the body's "insulin factory" - composed of pancreatic islet cells - is gradually destroyed by specialised white blood cells called "killer" T-cells which are defective.
But recently a team led by Denise Faustman, director of the Massachusatts general hospital's immunobiology laboratory and an associate professor of medicine at Harvard, found a way to isolate and eradicate this "killer" cells that are responsible for wiping out insulin-producing cells in the pancreas.The study, which will appear in the Proceedings of the National Academy of Sciences and has been released online, is the first demonstration of this strategy in human cells and supports the viability of a clinical trial that is currently underway.
They previously discovered a technique that reversed type 1 disease in a mouse model. "Our studies in mice showed that we could selectively kill the defective autoimmune cells that were destroying insulin-producing islets," says Faustman. "These results show that the same selective destruction can occur in humans cells and connect what we saw in our animal studies with the protocol we are pursuing in our Phase I clinical trial."
Faustman's team showed that triggering the expression of the immune-system modulator tumor necrosis factor (TNF) in diabetic mice led to the death of the T cells responsible for destroying insulin-producing pancreatic islets. After receiving this treatment, the animals were able to regenerate healthy islet cells that produced normal levels of insulin, effectively curing the animals' diabetes.
The current study used T cells from more than 1,000 patients with type 1 diabetes, other autoimmune disorders and healthy controls. First the researchers found that treatment with TNF killed CD8 T cells, the immune system's "killer" cells, from diabetic patients but not CD4 "helper" T cells. TNF treatment also induced the death of CD8 T cells from other autoimmune disease patients but had no negative effect on cells from healthy controls.
Even more, CD8 cells from diabetic participants that were targeted against two common viruses were not killed by exposure to the TNFR2 agonist, confirming that the protocol only leads to the death of T cells responsible for an autoimmune reaction.
The clinical trial based on Faustman's earlier studies is testing whether use of bacillus Calmette-Guerin (BCG), a generic drug that temporarily elevates TNF levels, will reduce autoimmune T cells in patients with type 1 diabetes. The current Phase 1 trial, which has been approved by the FDA and is directed by David M. Nathan, MD, director of the MGH Diabetes Center, focuses on determining the optimal dose and timing of BCG administration. More information on the 18-month trial, which began in March, is available at http://www.faustmanlab.org/.
Image Courtesy: Flint Buchanan/ngfn
17.09.2008