News • Post-transplant care
Improving heart transplant monitoring with molecular tests
Molecular testing is transforming post-transplant care, reducing the need for invasive biopsies and personalizing medication regimens to lower the risk of infection and other downstream side effects.

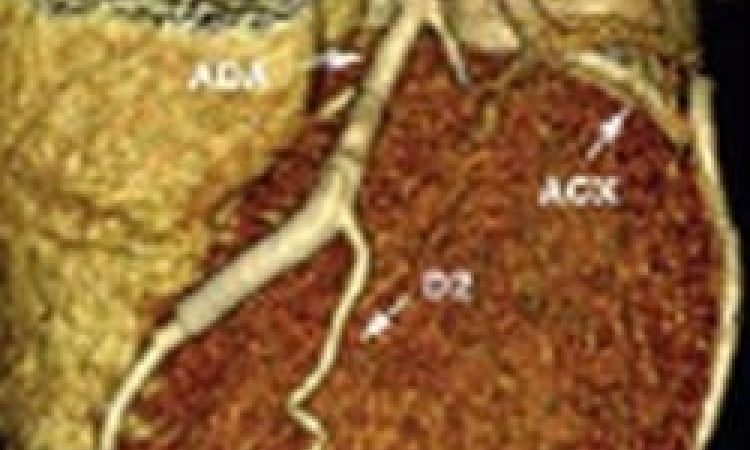
Image source: ISHLT
This is according to a presentation by Jeffrey Teuteberg, MD, at the Annual Meeting and Scientific Sessions of the International Society of Heart and Lung Transplantation (ISHLT).
“We’ve had a bit of a cookie-cutter approach to post-operative care, managing heart transplant patients in roughly the same way,” said Dr. Teuteberg, Associate Chief of Cardiology and Section Chief of Heart Failure, Cardiac Transplant, and Mechanical Circulatory Support at Stanford Medicine. “Besides addressing issues that come up for a specific individual, there hasn’t been a lot of personalization.”
Post-transplant surveillance has traditionally included frequent biopsies of heart tissue and blood tests for the first few years following the transplant when the risk of organ rejection and infection is highest. “Patients hate having the biopsies, but we haven’t had a good, non-invasive alternative,” Dr. Teuteberg said.
An early molecular test, gene expression profiling, made inroads by distinguishing between low- and high-risk transplant patients. Now, cell-free DNA (cf-DNA) testing, which identifies small DNA fragments in the bloodstream from a donor’s heart, can detect potential heart injury or rejection as early as a few weeks post-transplant. “When we started using cell-free DNA testing as early as a month post-transplant, we eliminated 95% of the biopsies during the first few years,” he said.
Being able to surveil patients remotely is more convenient for patients. I think it democratizes the heart transplant in a way that is really exciting
Jeffrey Teuteberg
Using cell-free DNA testing to monitor patient response holds the promise of enabling physicians to reduce the dosage of immunosuppressive medicines and steroids in low-risk patients. “Post-transplant medications keep the body from rejecting the donor heart, but they also can have deleterious health effects, including infections, impaired kidney function, and an increased risk for cancer,” he said. “Being able to decrease the dosage may benefit patients by reducing the incidence or severity of these complications.”
Molecular testing also offers the potential to:
- screen patients for viruses to personalize the duration of post-transplant antivirals and antibiotics
- test the patients’ own DNA to determine levels of viruses and bacteria in the gut biome, which may correlate with their level of immunosuppression
- detect early cancer cells to adjust screening rates for patients at high risk
- study gene expression in the heart tissue removed during biopsies.
Dr. Teuteberg said molecular testing is already improving access to heart transplants and quality of life for recipients. “One of the things that disadvantages patients who need a transplant is their ability to get to a transplant center, not only for the procedure but for ongoing testing,” he said. “Being able to surveil patients remotely is more convenient for patients. I think it democratizes the heart transplant in a way that is really exciting.”
While it’s difficult to quantify, Dr. Teuteberg said better surveillance of patients over a longer period of time could impact survival and outcome rates for heart transplant recipients. “Even if the impact is relatively modest, it would be a huge change because we haven't really been able to bend the survival curve beyond the first six months or a year despite all the great advances of the past 20 years,” he said. “If we're better at identifying who's at high risk of rejection and preventing that, it will have a huge tail in terms of the benefit over time. It doesn't take much of a change of the survival curve early post-transplant to have an impact on long-term survival,” Dr. Teuteberg said.
Source: International Society for Heart and Lung Transplantation
28.04.2025