Image source: Zhou et al., Lancet Planetary Health 2023 (CC BY-NC-ND 4.0)
News • Planetary health
Global analysis links antibiotic resistance increase to rising air pollution
Curbing levels of harmful air pollution could help reduce antibiotic resistance, according to the first in-depth global analysis of possible links between the two.
The research was now published in The Lancet Planetary Health journal.
Findings from the study highlight that controlling air pollution could greatly reduce deaths and economic costs stemming from antibiotic-resistant infections. The analysis indicates that increased air pollution is potentially linked with a higher risk of antibiotic resistance across global regions. It also indicates that the relationship between the two has strengthened over time, with increases in air pollution levels coinciding with larger increases in antibiotic resistance in more recent years.
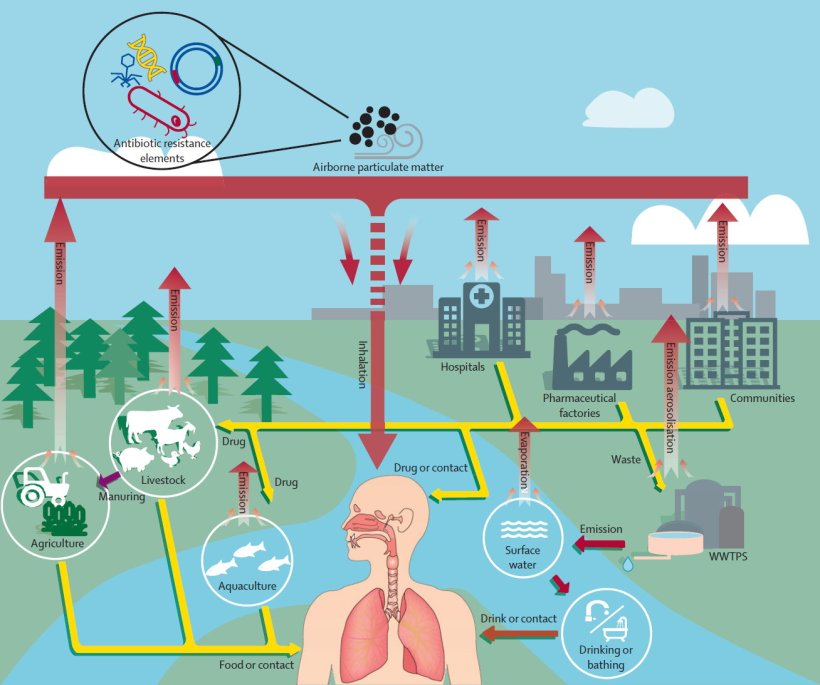
Although air is recognised as being a direct pathway and key vector for disseminating antibiotic resistance, there is limited quantitative data on the different pathways that antibiotic resistant genes are carried via air pollution. Some potential pathways include hospitals, farms, and sewage-treatment facilities that emit and spread antibiotic resistant particles through the air and across distances.
The benefits of controlling air pollution could be two-fold: not only will it reduce the harmful effects of poor air quality, it could also play a major role in combatting the rise and spread of antibiotic-resistant bacteria
Hong Chen
Lead author Professor Hong Chen, of Zhejiang University, China, said: “Antibiotic resistance and air pollution are each in their own right among the greatest threats to global health. Until now, we didn’t have a clear picture of the possible links between the two, but this work suggests the benefits of controlling air pollution could be two-fold: not only will it reduce the harmful effects of poor air quality, it could also play a major role in combatting the rise and spread of antibiotic-resistant bacteria.”
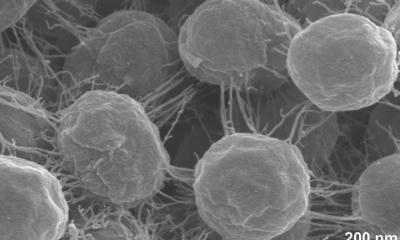
Misuse and overuse of antibiotics are the main drivers of antibiotic resistance, but evidence suggests air pollution also contributes to the spread of antibiotic-resistant bacteria and resistance genes. However, until now, there was limited data on how much influence PM2.5 air pollution – which is made up of particles 30 times smaller than the width of a human hair – has on antibiotic resistance globally. Sources of PM2.5 include industrial processes, road transport, and domestic coal and wood burning. Recent findings indicate 7.3 billion people globally are directly exposed to unsafe average annual PM2.5 levels, with 80% living in low- and middle-income countries.
The authors created an extensive dataset to explore whether PM2.5 is a key factor driving global antibiotic resistance, using data for 116 countries from 2000 to 2018. In total, data on more than 11.5 million test isolates were included in the analysis, covering nine bacterial pathogens and 43 types of antibiotics. Data on antibiotic usage, sanitation services, economics, health spend, population, education, climate and air pollution was used to investigate the influence of these factors on levels of antibiotic resistance. Data sources included surveillance databases, the World Health Organization, European Environment Agency, and the World Bank.
Recommended article

Article • Collection
Focus on environmental medicine
Harmful substances in the soil, water and air also endanger people's health. In recent years, environmental medicine has been increasingly concerned with the consequences of climate change.
The findings indicate antibiotic resistance increases with PM2.5, with every 1% rise in air pollution linked with increases in antibiotic resistance of between 0.5 and 1.9%, depending on the pathogen. The association has strengthened over time, with changes in PM2.5 levels leading to larger increases in antibiotic resistance in more recent years. The highest levels of antibiotic resistance are found in North Africa, the Middle East and South Asia, while levels in Europe and North America are low. Due to their large populations, China and India are thought to be the countries where changes in PM2.5 have the greatest impact on premature death toll from antibiotic resistance.
The analysis indicates antibiotic resistance resulting from air pollution is linked to an estimated 480,000 premature deaths in 2018. This led to additional economic costs of $395 billion.
The analysis suggests that PM2.5 is one of the leading factors driving antibiotic resistance, accounting for 11% of changes in average resistance levels around the world. In comparison, health spending accounts for 10% of changes, while drinking water services make up 3%. North Africa and western Asia are the regions where PM2.5 has the greatest impact on antibiotic resistance, where it accounts for 19% of changes to resistance levels.
The authors’ modelling of possible future scenarios indicates that if there were no changes to current policies on air pollution, by 2050, levels of antibiotic resistance worldwide could increase by 17%. The annual premature death toll linked to antibiotic resistance would rise to around 840,000, with the greatest increases in sub-Saharan Africa.
In other scenarios, such as increasing health spending, controlling air pollution, improving drinking water and reducing antibiotic usage, the level of antibiotic resistance could be greatly reduced. For example, implementing a policy – recommended by the World Health Organization – of limiting PM2.5 to 5 μg/m3 in the atmosphere could decrease global antibiotic resistance by 17% by 2050. This policy could lead to a 23% reduction in premature deaths (630,000 fewer deaths) linked to antibiotic resistance, and lead to annual economic savings of $640 billion.
The authors acknowledge some limitations to their study. A lack of data in some countries – particularly low- and middle-income countries, which are most affected by antibiotic resistance – may affect the overall analysis. Comparing results between countries should also be done with caution, due to differences in relative risks and the availability of testing. A key focus of future research should be on investigating the underlying mechanism of how air pollutants and other factors affect antibiotic resistance, and possible interactions between different factors.
Source: The Lancet
08.08.2023