Article • Institutional setup guide at SNMMI 2024
How to establish a hospital theranostics treatment centre
Report: Cynthia E. Keen
Nuclear medicine has been a stable radiodiagnostics imaging specialty, with few innovations until recently. In 2022, the nuclear medicine global market was valued at US $7 billion, according to market research firm MEDraysintell of Louvain-la-Neuve, Belgium. However, in nine years it is projected to reach US $39 billion, with 70% of the increase attributed to radiotherapeutics.
Theranostics was the topic of excitement at the annual meeting of the Society of Nuclear Medicine and Molecular Imaging (SNMMI) held June 8-11 in Toronto, Ontario. MEDraysintell predicts that numerous promising theranostic radiotherapeutic drugs are expected to be commercially available by 2028, with the majority targeting cancer treatments.
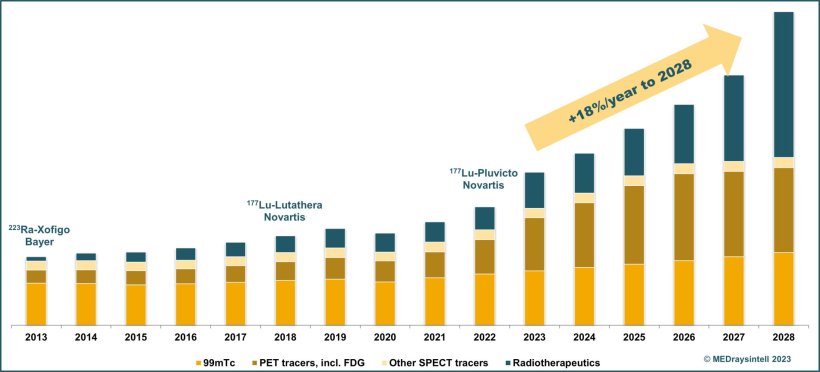
Image credit: Published in MEDraysintell Nuclear Medicine Report & Directory Edition 2023, courtesy of MEDraysintell
So how to set up a dedicated theranostics centre? An entire annual meeting session was dedicated to planning logistics, radiation safety, and waste management requirements.
“Skyrocketing” development
Dmitry Beyder, radiology program manager at Barnes-Jewish Hospital in St. Louis, Missouri, shared the “to do” checklist utilized by the nuclear medicine and radiation oncology departments to establish and launch the Center for Clinical Theranostica Research at the Mallinckrodt Institute of Radiology in September 2023. ‘Theranostics is a new field with the potential for exponential growth. It currently is a very expensive treatment for predominantly prostate cancer, but development of radionuclides proposed for other types of cancer and a variety of other diseases is skyrocketing,’ said Beyder.
But how to budget for this? In addition to capital funds, what hurdles does a dedicated center face to operate? Having an established, robust PET centre serving a large referral base is a good start. Beyder emphasizes that it is important to project the future. Vital questions for this are:
- What percentage of cancer patients in a given community does a facility currently treat?
- What percentage is referrals?
- What magnitude of growth is anticipated in the next 10 and 25 years?
- What theranostic drugs are currently approved, and for what types of treatment?
- Is there sufficient space for a dedicated centre? Is it large enough to support future growth?
- What will the design costs be?
- Can an existing hot lab be utilized or does a new or expanded one need to be built?
A typical theranostics treatment centre includes treatment rooms, toilets, a nourish/supply area, a radioactive waste room, a hot lab, and a work area for staff. The design must be patient-centric with an easy way to walk into and out of treatment rooms.
Need for aggressive staff recruiting
Projected staff requirements also need to be considered. These need to include physicians experienced in interpreting molecular imaging studies, medical physicists, certified nuclear medical technologists, a radiation safety officer, a clinical staff member to handle referrals, consultations, and complications, a radiochemist or radiopharmacist, a patient navigator, and support personnel.
Beyder pointed out that a shortfall of nuclear technologists is anticipated within five years in the United States and that not enough clinical staff interacting with patients will have the required nuclear medicine education. Therefore, expenses for aggressive staff recruiting and supplemental training must be incorporated in the budget.
The budget must also include the costs of hardware and software to support and grow the service, of radiopharmaceuticals, of adjunctive medications, of clinic supplies, and of staff salaries. Protocols and a system to evaluate patient eligibility must be established. Reimbursement payments must be estimated.
Finally, several strategic questions should be taken into account:
- Is the hospital willing to make the investment if the theranostics centre cannot support itself?
- If so, how long can it support losses?
- And finally, will it meet the SNMMI standards to be a Comprehensive Center of Excellence?
Radiation safety and nuclear waste considerations
If a person has to use a toilet that is at the end of a long hall, he or she could cause contamination that could affect and shut down the entire department. Patients urinate out 50% of the radiation dose they received within five to six hours
Kyle Underwood
Kyle Underwood, a Certified Health Physicist specialising in radiation safety at Mayo Clinic in Rochester, Minnesota, discussed radiation safety planning when setting up a theranostic centre.
Working with a design team at the outset of planning is critical to plan radiation shielding for both public and controlled areas, and that the space must be very carefully designed to minimize accidental contamination. ‘It is very important to minimize the amount of walking that a patient has to do to get to a WC. If a person has to use a toilet that is at the end of a long hall, he or she could cause contamination that could affect and shut down the entire department,’ Underwood cautioned. ‘Patients urinate out 50% of the radiation dose they received within five to six hours. Some infusions take hours to complete.’
Lead shielding requirements will be minimized if patient treatment rooms are located side-by-side. Large treatment rooms are not feasible unless there is a need to minimize lead, because when one is contaminated, it can take up to an hour longer to decontaminate than a small room.

Image credit: Courtesy of Vikas Prasad MD, PhD, Washington University School of Medicine in St. Louis
Good room preparation pays off later
A large radiation waste room that can accommodate a contaminated patient bed rolled into it is recommended. ‘If you have a patient who is incontinent and voids into a bed, from a centre’s workflow perspective, it may be more optimal to spend less time cleaning the room by rolling the bed into the radiation waste room and decontaminating it later,’ suggested Underwood.
A bed should have multiple layers: a fitted top sheet, with a plastic sheet underneath, followed by an absorbent pad sitting on a fitted sheet. A paper walkway taped to the floor from bed to bathroom minimizes urinary dripping cleanup. A toilet should have full taped down plastic protection, surrounded by floor-to-ceiling plastic sheeting to contain splatter. ‘Room preparation against patient contamination or a leaking infusion line can be expensive and time consuming, but if you have a bad day with a patient, it more than pays for itself,’ he said.
The rule of thumb for releasing a patient to self-isolate at home is at less than 500mg dose of radioactive pharmaceuticals. Patients need to be admitted as inpatients if greater, and require a private room, a private bathroom, radiation safety placards, and treatment of all trash as radioactive waste. Everything that leaves the patient’s room must be surveyed for radioactive contamination by a radiation safety officer. Anyone entering the room must be trained in radiation safety procedures. Inpatients receiving treatment require the same guidelines.
Profiles:
Dmitriy Beyder is a Radiation Program Manager at Barnes-Jewish Hospital in St. Louis, MO. He was a member of the team to establish the Center for Clinical Theranostics Research at the Mallinckrodt Institute of Radiology at Washington University School of Medicine in St. Louis. Beyder is also the current president of the Technologist Section of SNMMI.
Kyle Underwood is a Certified Health Physicist at Mayo Clinic in Rochester, Minnesota. He leads multiple unique modality teams to provide excellent staff safety and patient care. Of particular interest is radiation protection and the treatment of diseases with existing and novel radiation therapies.
09.07.2024