ElastoScan in breast ultrasound
Dr Katja Gabriel of the Hirschhauser & Gabriel Obstetrics and Gynaecology Practice in Erkrath, Germany, describes clinical experience with this novel technique and the resulting improved diagnostic accuracy.
In recent years, breast ultrasonography has become an essential procedure in the diagnostic evaluation of breast tissue. The improvement in ultrasound technology, particularly the high resolution of modern devices and the use of colour Doppler sonography, has made this technique indispensable in daily routine.
Although several studies have proved the value of conventional breast ultrasound, there are still a growing number of patients who undergo unnecessary breast biopsy even when techniques such as ultrasound, mammography and MRI are combined. The use of ultrasound elastography appears to enhance diagnostic accuracy by visualising tissue elasticity. In breast examination, the assessment of lump rigidity has usually been carried out with normal palpation. It is well known that malignant lesions are generally harder than benign lesions. Therefore, elastography appears to increase the sensitivity and specificity of breast ultrasound.
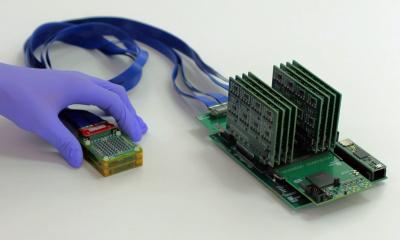
In the examples shown, ultrasound examination was performed using the Sonoace Accuvix V20 Prestige system. Real-time elastography using ElastoScan was performed with a 5-13 MHz linear transducer. Most of the women underwent the examination for screening purposes; however, some were examined because of a palpable breast lump or on routine followup after breast cancer therapy. Each breast was examined lesions were carefully assessed using the following standard criteria: shape, margin, orientation, lesion boundary, echogenic pattern, posterior acoustic features, the effect on surrounding tissue, calcifications and vascularisation using colour Doppler. They were then classified according to the BI-RADS score. This standard approach was immediately followed by the elastographic examination. For this purpose, the transducer was not moved from the previous position and only slight pressure was applied. The colour map 4 was used with red indicating soft tissue or fluid and purple indicating hard tissue.
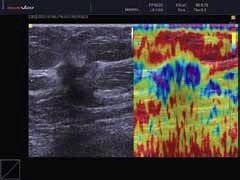
Figure 1 shows the breast screening ultrasound scan of a 47-year-old female. The lesion was non-palpable, 14 x 13 x 11 mm in size, irregularly shaped, hypoechoic with indistinct margins. There was posterior shadowing, disruption of surrounding tissue architecture and suspicious adjacent vascularisation. The lesion was therefore classified BI-RADS V. The ElastoScan revealed the tumour stiffness, indicated by blue to purple colour in contrast to the soft surrounding fibroglandular and fat tissue indicated by red and yellow. This information not only supported the suspicion of malignancy, but also contributed to the identification of the tumour boundaries, indicating a wider tumour expansion laterally, but not posteriorly. Core needle biopsy revealed invasive-ductal carcinoma.
Figure 2 is a scan of a 60-year-old woman with macromastia and status post breast surgery with extirpation of a fibroadenoma. There was a diffuse hypoechoic area. The ElastoScan revealed the softness of the tissue indicated by yellow and red colour. Therefore, with knowledge of the patient’s history of surgery, the changes were attributed to post-operative scarring. This was supported by mammography. No core-needle biopsy was performed.
Figure 3 depicts the scan of a 57 year-old female with mastodynia. There was a nonpalpable hypoechoic lesion of ovaloid shape with only discretely irregular margins, horizontal orientation, distinct boundaries, posterior enhancement and no calcifications or suspicious vascularisation. The lesion was classified BI-RADS II. The ElastoScan showed yellow and red colour of the lesion and yellow and blue colour of the surrounding fibroglandular tissue supporting the benign aspect. The lesion was classified BI-RADS II and therefore biopsy was not required. A growing number of studies indicate the diagnostic value of elastography when added to conventional breast ultrasound. Especially in BI-RADS III lesions, an elastogram that shows relative softness can be reassuring and thus prevent unnecessary breast biopsy. Our clinical experience shows, that ElastoScan is easily conducted and gives results instantaneously. Elastography should always be used in combination with conventional ultra-sonography and further studies n ed to be done to show the sensitivity and specificity of the technique. In the future, elastographic findings should be included as an independent criterion in the BI-RADS score. Although webiopsy in BI-RADS IV conventional ultrasounds, even if the ElastoScan shows softness, we will continue to use it in order to support our breast ultrasound diagnosis and in many cases to reassure our anxious patients.
SONOACE is at MEDICA
Hall 9. Stands B60-1 and B60-2
18.11.2011