Article • Radiation management
'Dose hysteria' and the 320-slice CT scanner
Sometimes radiation dose is a topic discussed hysterically. Dose discussion is necessary, but should be carried out based on the highest levels of knowledge and seriousness.
By Dr Patrik Rogalla, Senior Consultant at the Charité, Berlin
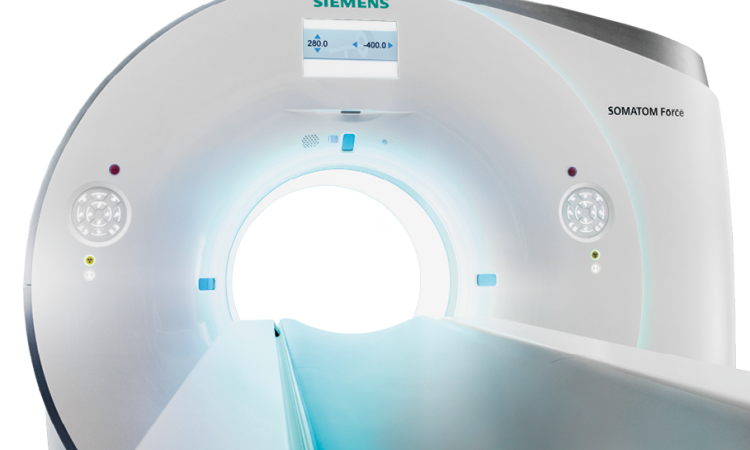
For the last few months, Dr Patrik Rogalla, Senior Consultant at the Charité, Berlin, specialist in diagnostic radiology and Head of the Computed Tomography Department at Campus Mitte, University Medicine Berlin, has been using a 320-slices CT scanner, one of 51 currently manufactured. During our interview, we asked whether the system has provided greater detection rates, and why it has also ignited further debate on radiation dose.

‘Radiation dose is a topic that is sometimes discussed rather hysterically, and often by many without sufficient basic knowledge on the subject. Reason number one: if people are short on interesting and innovative topics they will talk about radiation dose. This always goes down well and scores points, because radiation is generally perceived as something very negative in our society. Once you tackle this topic you are guaranteed to remain a talking point. The second reason: Of course we must cut down on dose and are obliged by the legislators to examine using the lowest possible dose. The reason why the 320-slices is re-igniting discussions is the potentially lower dose requirement of this new type of CT scanner, and this puts us into the focus of the discussions around dose.
‘There are not quite so trivial discussions around the question of how much dose is required for what kind of image quality. The dose can be measured – it is not that easy but technically it can be done in a fairly reliable way. However, image quality can only be conditionally objectively measured, because a large part of image quality is determined by subjective impression. The real measure should be: How much of a dose do I need for a sensible image quality that allows safe diagnosis? However, seeing how images tend to make very subjective impressions, this opens the floodgates to all kinds of speculation and marketing. CT scanners manufactured by all the main suppliers all require a certain degree of a radiation dose for comparable examinations. The differences between the different manufacturers are rather marginal. The parameter setting of the equipment, determined by the radiologist based on the individual requirements of a patient, and in particular the clinical question at hand, is much more important.
No new drug, no new examination procedure would ever become market-ready these days if the risk evaluation was carried out without such a lack of solid, scientific base as the discussion around dose in radiology
Patrik Rogalla
‘It is a little regrettable that the discussion about CT tends to be reduced to a discussion around dose, although the use-risk ratio of CT scanning across medical indications is calculated at around 200:1. This is not only damaging for this technology, but also for radiology itself. This discussion then questions many radiological procedures, such as conventional angiography and fluoroscopy. How can you convince a female patient to have embolisation of a fibroid carried out using fluoroscopy when there is this constant debate over the dangers of radiation during CT scanning? We are taking away our own basis for essential methods of examination and treatment in radiology. I think this is short-sighted. The discussion around dose is necessary, but should be carried out based on the highest levels of knowledge and seriousness. One of the great difficulties with this discussion is that in today’s scientific world, where you cannot refer back to publications from Medline going back more than 4–5 years, nobody can be bothered to carry out proper research into data on exposure to radiation in the way it is required. A piece of research carried out two years ago is referred to because it appeared in a “respectable” journal, and is used as proof that radiation has a “calculable” risk. However, when you take a closer look at this piece of research you then see that it, in turn, refers to another piece of research carried out a few years previously, and this in turn quotes another piece of older research, which eventually takes us back to the original source – data from those who survived Hiroshima. Apart from very few exceptions, these survivors’ data are thus the only source – and of course they don’t constitute a scientific study but consist of estimates and observations – observations of a disastrous situation following the dropping of an atomic bomb. This source – and luckily we have not had to experience a more recent, comparable event – is used to deduct a seemingly high degree of evidence, recalculated over and over again and used as hard data to calculate literally the deaths per examination rate, although the basic data hasn’t changed and the linearity of radiation damage to dose remains a hypothesis. No new drug, no new examination procedure would ever become market-ready these days if the risk evaluation was carried out without such a lack of solid, scientific base as the discussion around dose in radiology.’
Recommended article

News • Radiation protection
Is contact shielding during X-rays, CT scans obsolete?
The British Institute of Radiology (BIR) and a working party of UK radiological professional bodies and agencies have published evidence-based guidance which shows that patient contact shielding (such as aprons, thyroid or gonad shields) provides minimal or no benefit. It concludes that there are other areas of radiation protection which are more effective in optimising radiation exposure such as…
Dr Rogalla is currently using a dynamic volume 320-slices scanner. ‘This refers to the term dynamic imaging in general,’ he explained. ‘Dynamics is a process that stretches over a period of time and as such can be captured. This can be movement, perfusion, blood flow or a metabolic process. Previously CT diagnostics was more or less like picture taken with flashlight; the freezing of a moment. However, dynamic imaging captures the course of a process.
‘If you handle dynamic CT imaging wrongly then dose can really become a problem. But we have enough ways around this to avoid that problem. You can distribute the dose across a period of time, literally fraction it. We line up several images one after the other, each of which obviously only requires a fraction of the whole dose, so that the entire dose during an examination of several seconds or minutes remains the same. We compensate for the resulting image loss with mathematical solutions – by averaging over time using new filters. This works. It involves one of the concepts of post-processing; admittedly, this is still under development. I am convinced that we will see very interesting new approaches to solutions during the next scientific congresses.’
02.11.2008