Achieving HbA1c target values
Report: Karoline Laarmann
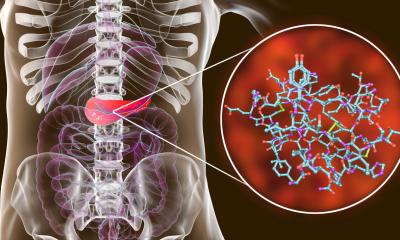
An adequate blood glucose level (4–7 mmol/l) is important not only for a diabetic’s daily well-being but also to prevent diabetes-related illnesses. HbA1c is the central marker to evaluate the success of diabetes management. But HbA1c measurement has a crucial limitation: current blood glucose fluctuations are not taken into consideration. However, the recognition of steep post-prandial blood glucose increases is important to prevent extreme phases of hypo- and hyperglycaemia.


Intermittent regular self-monitoring of blood glucose (SMBG) helps patients with Type 2 diabetes to achieve the desired HbA1c target value and catch and counteract glucose fluctuations. Moreover, the guidelines Self-Monitoring of Blood Glucose in Noninsulin-Treated Type 2 Diabetes (pub. 2009, by the International Diabetes Federation), confirm that even Type 2 diabetics who do not take insulin benefit from SMBG. This is a remarkable signal because, so far, decreasing HbA1c has not been considered clinically relevant for this group.
According to Professor Oliver Schnell, Executive Member of the Managing Board and Head of the Department of Diabetes and Cardiovascular Disease, Diabetes Research Institute, Munich, therapy adjustment for Type 2 diabetes should focus on blood glucose measurement rather than on HbA1c, no matter whether the patient takes insulin or not. ‘Glucose fluctuations, average pre-prandial, post-prandial and nocturnal blood glucose levels, decrease with intermittent SMBG,’ he adds.
Speaking at the 45th annual meeting of the German Diabetes Society, held in Stuttgart, Prof. Schnell presented promising results of the Accu-Chek 360° View study, which looked at structured blood glucose measurement.
522 non-insulin using Type 2 diabetics (HbA1c > 7.5%) participated in the prospective, cluster-randomised study, conducted for one year at 37 sites in the USA. Patients in the intervention group received in-depth training on the use of SMBG data. Therapy adjustments were based on quarterly tests (seven measurements in three consecutive days). However, in the control group HbA1c changes were the prime target parameter.
‘While HbA1c had been similar in both groups at the outset of the study, already in the first six months the HbA1c value in the intervention group was 0.35% lower than in the control group,’ Prof. Schnell said. Treatment modifications and lifestyle changes were much more frequent in the intervention group (over 80% of the patients). ‘Best outcomes were achieved in the adherent intervention group: the patients who recorded their daily blood glucose levels, who were physically active or changed their nutrition, had HbA1c values that were 0.43% lower than those in the control group.’
Further, SMBG seems to positively impact on diabetes-related emotional stress, the professor emphasised. ‘The concern that SMBG exacerbates depression symptoms and emotional stress is entirely unfounded. The more responsibility diabetes patients are given in their disease management, and the more they learn about their disease, the better they handle it.’
14.07.2010