Ultrasound wins role in chemotherapy assessment
Step-by-step, ultrasound is advancing as an alternative for determining whether a cancer patient’s treatment is working or should be changed. Not everyone welcomes this disruptive new approach, John Brosky reports.

Ultrasound has always been treated as an orphan child in radiology. It is readily available, highly portable, non-invasive and non-radiating. With a certain level of training, ultrasound can be used by anyone in the hospital. Which is why radiologists increasingly see ultrasound as a threat to their role in the medical community. On the low-end of its capabilities, ultrasound today is rapidly replacing the stethoscope as the first tool of choice for routine examinations. On the high-end, thanks to the same increase in processing power that generates startling diagnostic images for CT and MRI, enhanced ultrasound delivers dynamic images in four dimensions that have won the highest recommendations in guidelines across multiple pathologies.
Similarly, the recent availability of a contrast agent for ultrasound now enables perfusion studies, an assessment of blood flow in organs that, unlike static scanner images, show real-time flow, illuminating the function of organs for physicians – all this presenting neither radiation nor the introduction of toxic or radioactive chemicals.
The quality of ultrasound images has won the begrudging support of radiologists. Now their last objection, that ultrasound cannot be relied upon for quantification, is being successfully challenged. This year cardiac ultrasound won the highest recommendations from European cardiologists for the assessment of valvular heart disease, including the measurement of the annulus, a critical parameter for repairing or replacing the valve.
In oncology, a new study is breaking down barriers, winning validation for techniques to measure changes in tumours, to this point considered to be the exclusive province of radiologists with their big metal scanners. There are competing gold standards for response evaluation criteria in solid tumours (RECIST). Depending on the type of tumour and its location, either CT or MRI is required. A rules-based evaluation can determine whether cancer patients are responding to chemotherapy, are unchanged or worsening. This diagnosis is crucial for oncologists to determine the next step in treatment.
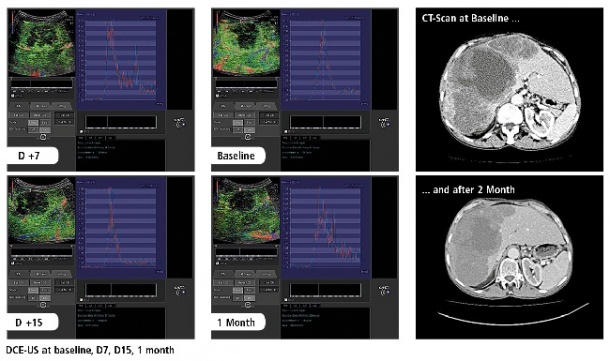
While tumours can be seen with ultrasound, no one was able to reliably measure changes to the tumour. In 2010, Nathalie Lassau from the Institute Gustave-Roussy in Paris led an effort to determine whether using a contrast agent, as with CT and MRI, a perfusion study of tumours using ultrasound could assess changes as a result of chemotherapy. The short answer is that it is not only possible and reproducible, but also the exam costs less than €200 and can determine, faster than scanners, whether a treatment is working or should be changed. (European Hospital 2/2011) Identifying non-responders in the first month of treatment could prevent patients from enduring a further five months of treatment and save healthcare systems an estimated $40,000 per patient.
Building the case for ultrasound RECIST
With the first wave of scientific work behind her and a solid clinical trial in her portfolio, Dr Nathalie Lassau has been on the road presenting the case for ultrasound RECIST across Europe, North America and Asia. European Hospital caught up with her at the French Radiology Congress in Paris, where she announced that the final study, Standardisation of Dynamic Contrast-Enhanced Ultrasound for the Evaluation of Antiangiogenic Therapies, is to be published in November 2012, in Investigational Radiology.
Dr Lassau is also travelling to the Radiological Society of North America meeting in Chicago to present her preliminary studies demonstrating tumour quantification using 3-D transducers for a three-minute exam that enables interventionalists to be sure all of a tumour is targeted. Returning to the break-through study she said, ‘What we proved, is that by following patients we were able to determine the best parameter to measure, using contrast-enhanced ultrasound. We showed that, with this measure, within one month of treatment if a patient does not show a diminution of 40%, the treatment should be changed.’
The study followed 539 patients over one year at 19 oncology centres in France for a total of 2,339 exams using a technique called Dynamic Contrast Enhanced Ultrasound (DCEUS). The raw linear data from each exam were transferred from the different sites to the main study centre at the Institute Gustave-Roussy for quantitative analyses. Aware that the eyes of the radiology community would scrutinise every aspect of the study, Dr Lassau said both the trial and the resulting publication are severely methodical.
Only 4% of the exams had to be excluded
A secondary finding of the study was that, after 60 exams or approximately two months, a sonographer could reliably perform the exam. ‘This means it’s a technique that can be shared throughout a hospital centre,’ she said, adding that the evaluation software has been validated so that data does not need to be sent to Paris for analysis. ‘It takes just a few seconds to quantify the exams,’ she said. To date, 65 radiologists have been trained to use the technique, which this summer was included in the ‘Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound, published by the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB).
Crucial to the study was the ability to obtain pure ultrasound signal data for mathematical modelling. Only Toshiba was willing to release its signal data for the study and the company continues to work with Dr Lassau’s team as the project has expanded. The software developed by the Institute Gustave-Roussy has been licensed by Toshiba and integrated on its Aplio ultrasound platform. Dr Lassau also said she is now collaborating with Toshiba engineers in Japan on her next frontier in RECIST quantification using ultrasound, the 3-D evaluation. ‘It is a technical challenge,’ she said, ‘ but that’s research!’
12.11.2012