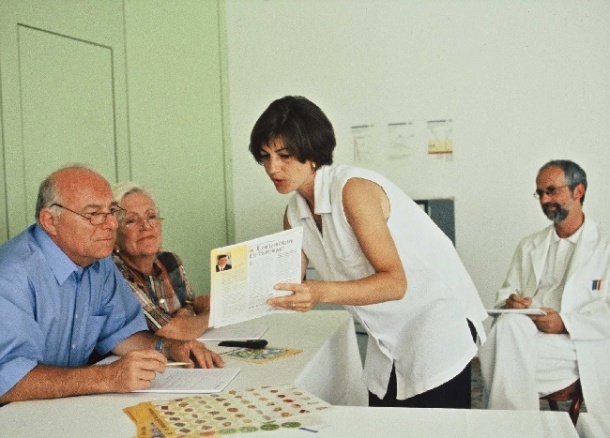
Study shows nurses taking charge of diabetes care in hospital means more patients hit target glucose levels
A nurse-initiated, nurse-led, and nurse-implemented study shows that nurses taking charge of diabetes care in hospital results in more patients hitting their target glucose levels. The study was led by Esther Boteach, Soroka University Medical Center Beer-Sheva, Israel, and co-workers.

Previous work has shown greater mortality and morbidity among hospitalised diabetic patients compared with non-diabetics. Patients without previously diagnosed diabetes that are hospitalised with high glucose have mortality three times higher than known diabetics and 10 times higher than the general population. The “sliding- scale treatment regimen ", still frequently used in many hospitals based on a fixed dose of regular insulin for a given level of glucose has failed in achieving glucose control in the hospital setting. Boteach and colleagues proposed the Glucose Control In the Hospital Project, using the basal-bolus approach—this approach has been shown to achieve better glucose control. Long-acting basal and meal time short-acting analogs were used according to the protocol algorithm. However, effective implementation this protocol requires easy to use, effective algorithms and education of all medical and nursing staff. Additionally, hospital kitchen staff must adjust carbohydrate content of meals to match the protocols.
The project took place in the 1000-bed Soroka University Medical Center, Beer-Sheva, Israel, which serves a multi-ethnic, multi-cultural population of close to one million people. The programme had a number of elements: 1) Education and update of all staff, including doctors, nurses, all ancillary ward staff, and kitchen personnel on the importance of hospital glucose control. 2) Specific training courses for nurse diabetes managers for each ward. 3) Basal-bolus and intravenous (IV) insulin protocol generation for glucose management and control. 4) Changes in food preparation and delivery, including preparation of standard menus for diabetes patients.
Within one year 500 doctors, 1,100 nurses, 20 pharmacists and 200 ancillary staff had participated in the project. The protocols have been implemented by nurses in 17 of 26 wards to date. The proportion of patients reaching a pre-set fasting plasma glucose target of (5.5-6.7 mmol/l) went from 18% prior to the implementation to 40% post implementation, and the post-meal target (7.8-10mmol/l) was achieved by 21% prior to and 49% post implementation. The mean daily dose of insulin increased from 7.5 to 16.3 units/day and mean glucose concentration decreased by 28%. Most nurses asked (95%) agreed that the project significantly improved the treatment of people with diabetes, while 82% thought that cooperation with doctors improved, and 95% stated that implementation of the protocol by nurses had decreased nurses’ dependence on doctors and empowered nurses professionally.
“A nurse-initiated, nurse-driven and nurse-implemented comprehensive program for the management o diabetes in the hospital is feasible, doable and successful,” conclude Boteach and co-workers.
Picture Credit: Lilly
22.09.2010