PACS: the never ending story
A short story about life with and without PACS written at the University Hospital for Radiodiagnostics.

Helga Fischer, radiographer at the University Hospital for Radiodiagnostics at the Allgemeine Krankenhaus, Vienna, and former Vice-President of Austria’s RTA Association, which focuses on MR, lectures and workshops for imaging processes, describes experiences, covering a year and a half, with a PACS system, and suggests ways forward.
Once upon a time, in Vienna, a radiologist worked with a group of sweet tempered radiological-technical assistants (RTA), making many, many X-rays of many patients. The assistants prepared the X-rays on the light board, where after scrutiny, the radiologist prepared the diagnosis. The typing pool was so busy writing reports of the findings that their fingers went numb. Only after reports were typed were patients allowed to collect their X-rays and reports at the office. When needed, the referring physician was given the reports and X-rays. Lots of other people - e.g. mailmen and archivists - searched for and distributed large bags of reports and letters. Everyone lived happily, until PACS destroyed this heaven on earth ...
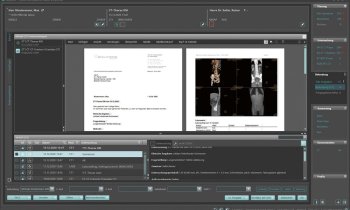
In October 2003, a PACS - AGFA’s IMPAX combined with a RIS by Siemens (Magic SAS) - went into routine operation at Vienna’s University Hospital for Radiodiagnostics at the Allgemeine Krankenhaus. IMPAX is an application that runs on UNIX servers and includes a list of advantages (a central database, all examinations saved in one system) and disadvantages (very complex and not always the desired response time).
Presently PACS has been partially implemented in three of the clinics:
• university hospital for radiodiagnostics
• trauma surgery
• X-ray therapy
Over 70 modalities are connected to the PACS network. In addition, approximately 30 diagnostic stations with two flat screens each (resolution between 1 and 3 mega pixel) are also installed in the hospitals.
The layout of the PACS is designed and dimensioned to include:
• Images saved in the short as well as long-term archive after acceptance by the server.
• The short-term archive allows relatively fast loading of archived images.
• The long-term archive is designed for 10-year storage. Data are only rarely retrieved.
• Pre-fetching should mainly take place from the short-term archive.
• •For security reasons, data must be present at least twice, whereby one copy should be stored ‘remotely’.
Present workflow - This practically depends on people and the ‘green folder’, a collective folder used to transport all findings, images, language cassettes and task lists for the examinations. The RIS and PACS are presently used as passive systems.
Even though workflow is presently very smooth, there are three sources for errors and time-consuming complications:
Time pressure at central planning - Because processes at central planning are so fast but the IT input does not happen synchronously (capture KIS - RIS), the patient index numbers are written manually.
Transfer of the worklist to modalities - There is no consistent transfer of the electronic work list from RIS to the modalities (they are older models). All relevant data must be entered manually particularly for the older modalities, which is a potential source for errors.
Diagnostic findings - The diagnostic process (dictation, writing, proof-reading, corrections and revision) and particularly the interaction between doctors and the typing-pool, is clearly a source for errors and there’s a potential for time optimisation.
Since PACS arrived, what are the most important disadvantages and advantages?
Disadvantages
• MTRA was not integrated into selection and purchasing process
• Selection, purchasing and implementation took too long, so when the system effectively went into operation, it was already too small
• When pictures are printed from PACS (e.g. CT) and the person involved does not ensure the printer is at the right level, all pictures may be printed twice (expensive)
• When there is a problem within the IT system, the complete PACS system goes down
• Under certain circumstances, images that are sent to the PACS are not saved in the right place; in which case the IT specialist must reprocess
• Retrieval of master images from the main storage can take up to hours; the IT specialist must be contacted
• Data must be entered absolutely correctly when an examination takes place in rooms where a patient’s data cannot be transferred into the examination computer, otherwise the images cannot be found in the PACS; the technician must reprocess in these cases
• High service and maintenance costs
• Display is monitor-dependent
Advantages
• Waiting times for the patients have reduced significantly
• Examinations can start more promptly
• Increased patient frequency is possible
• There is reduced film development and thus fewer toxic developing substances
• Lower film costs
• Better quality, as images can be saved digitally without losing data
• Better availability for diagnostic findings, visits or interdisciplinary consultations.
Overview - At present the PACS has stored about 8,897,000 images (files) with some 5,308 GB (raw) total data volume.
Computed tomography
• 25,450 CT exams
• average 238 images per picture
• approx. 6 million data files
Magnetic resonance
• 10,494 MR exams annually
• average 247 images per picture
• approx. 2.5 million data files
Additional modalities
• 248,400 data files from gastro, bones, etc.
In view of these volumes, the short-term archive (magneto-optical disc) will be filled within two years. Consequently, the oldest storage media must be removed from the library at regular intervals and replaced by blank ones.
Suggestions for improvement
Our wish list:
• The permanent employment, in the hospital, of a contact for doctors and IT people, who is capable of developing the most important IT strategies for the individual IT and medical-technical projects (such as PACS, RIS, KIS). This will ensure realisation of the intended synergies, consolidation and conformity for the systems.
• The nomination of a project manager from within the department/hospital, for a large and complex project such as PACs, the implementation of which takes several years and possibly longer. This person should be the connection between the hospital (professors, doctors, RTAs), and IT and manufacturer, and should be accepted as such by all those involved.
• The nomination of someone from the department/hospital, to take care of various IT-specific tasks. Experience in other hospitals clearly prove that this position is a prerequisite: It should not directly include the implementation of IT projects, but aspects such as:
- cooperation with IT, manufacturer, medical technology and doctors
- Training involving the IT user systems, such as RIS and PACS
- First contact person regarding IT-relevant questions for doctors and RTAs
- Constant training for new doctors as well as RTAs, for various IT systems, so that these are actually used consistently.
... and thus I would like to end our PACS story, but it’s nowhere near finished.
Finally, I would like to express my gratitude to: Mr Weigl MA, and his team at Consulting AIMC, whose help enables us to accomplish the impossible.
07.08.2006