Image source: Shutterstock/Maridav
Article • Covid-19 disinfection
New insights into SARS-CoV-2 surface stability and temperature susceptibility
Surface disinfection has proved an effective method to control Covid-19 infection, as virologists from the Ruhr University Bochum (RUB) have shown. However, an effective disinfection strategy against Coronavirus must consider various factors, says Professor Eike Steinmann. The head of the Department of Molecular and Medical Virology at the RUB explained when disinfection is an effective procedure against SARS-CoV-2, which agents are suitable to inactivate the virus and why private individuals should not reach for the ‘strong stuff’ without good reason.
Report: Wolfgang Behrends

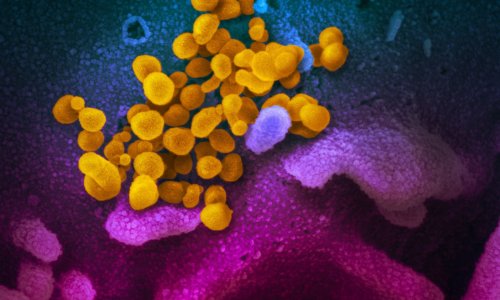
Whether or not a disinfectant is effective against a certain type of virus depends, among other reasons, on the structure of the virus, Steinmann explains: ‘Coronavirus is covered by a lipid membrane which stores proteins. This makes it susceptible to alcohol-based disinfectants because they destroy the membrane and inactivate the virus.’ If this membrane is missing, as, for instance, is the case with norovirus, other agents need to be used for disinfection.
The use of UV radiation has proved effective against such non-enveloped types of virus because it attacks the nucleic acids (RNA) of the virus. In concrete terms, this means that agents classed as having a limited virucidal effect are perfectly adequate for the inactivation of Coronavirus SARS-CoV-2. However, as more resistant agents, such as the aforementioned norovirus, are also present in a clinical environment, the use of more potent agents (classed as ‘virucidal’ or ‘limited virucidal plus’) may also be of benefit.
Effective disinfection should be carried out on all surfaces which have potential contact with the virus: work surfaces and surfaces close to patients, beds, and medical equipment. Current studies on SARS-CoV-2 confirm the presence of the virus – or at least its RNA – in many locations in a room where an infected patient had been accommodated: the edges of the bed, light switches, door handles, but also toilet seats, remote controls and pillows. ‘This shows that the virus is spread almost everywhere in the room via contact with hands as well as through the smallest droplets,’ Steinmann says. ‘However, thorough cleaning and disinfection can reliably deactivate the virus.’
Laboratory lifespan of SARS-CoV-2 gives indications
The virus was still present on the inside of masks after 7 days
Eike Steinmann
One of the central issues which researchers worldwide are examining concerns the lifespan of the new coronavirus on surfaces. Whilst initial calculations are mainly based on experience with the related virus types SARS-CoV and MERS-CoV, newer studies provide reliable figures on Covid-19 pathogen SARS-CoV-2: ‘One study, published in the New England Journal of Medicine, is of particular interest,’ says Steinmann. ‘US researchers examined for how long the virus survived on different materials, including copper, carton, steel and plastic surfaces. The results showed that in some cases, the virus is still present and active after several days. Everyday items such as banknotes, handkerchiefs and masks were tested in another study published in the Lancet Microbe: ‘The virus was still present on the inside of masks after 7 days,’ says the virologist and adds: ‘Although these measurements were taken under laboratory conditions, they give us a pretty good idea of how long the virus can remain stable in everyday conditions.’
Recommended article

News • COVID-19 longevity
How long can the coronavirus persist on surfaces?
How long can coronavirus persist on surfaces such as door handles or hospital nightstands? How can the virus be destroyed effectively? A research team from Greifswald and Bochum, Germany, collected the answers scientists can currently offer to these and other pertinent questions and published them in the Journal of Hospital Infection.
What role does temperature play?
Currently, researchers at the RUB under Junior Professor Dr Stephanie Pfänder are examining the effect of changes in room temperature on the lifespan of the virus. Scientists compared the surface stability of the virus at room temperatures of 4°C and 30°C. They found that the virus remains infectious on surfaces for roughly the same length of time in both hot and cold conditions. ‘The assumption had been that higher temperatures would lead to a lower transmission rate of SARS-CoV-2 in summer,’ says Pfänder. ’However, it appears that the stability of the virus on surfaces is not impacted by changes in temperature.’ A potentially lower rate of infection in summer could be due to other factors such as UV radiation and humidity though, says the virologist.
'Less is more' in private households
If you have a disinfectant at home, it makes you feel safe just in case. The actual use is then not actually that important
Eike Steinmann
Steinmann emphasises that there should be different criteria for private households as opposed to hospitals: ‘In everyday life, normal hand washing – combined with social distancing and following the correct coughing etiquette – is usually completely sufficient. Disinfection is only required once there has actually been contact with an infected person.’ Steinmann explains, in terms of the explosive demand for disinfectants amongst private individuals as follows: ‘In many cases, this will have been impacted by a psychological effect: If you have a disinfectant at home, it makes you feel safe just in case. The actual use is then not actually that important.’
If private households reach for the ‘strong stuff’, i.e. a disinfectant, they may not be doing themselves a favour, warns the expert: ‘These agents are aggressive and can attack the skin if used regularly.’ Without comprehensive care, this can easily result in skin injuries.
Profile:
Professor Eike Steinmann has been head of the Department of Molecular & Medical Virology at the Ruhr University Bochum since 2018. After completing his degree in biology at Hanover University and Northeastern University, Boston, USA, he completed his doctorate at the Institute of Molecular Virology at Heidelberg University. Steinmann then became a research associate and junior group leader in the Department of Experimental Virology at Twincore - the Centre for Experimental and Clinical Infection Research in Hanover. In 2012, he wrote his habilitation in Experimental Virology at Hanover Medical School, and from 2014 he managed the working group on ‘Virus Transmission’ at TWINCORE. In 2016, he was appointed ’Adjunct Professor’ at Hanover Medical School.
24.09.2020