Article • Precision imaging
Myth or reality? Focusing on personalised radiology
With precision imaging playing a greater role in daily radiology practice as patients receive ever more personalised care, the detail and extent of that shift is outlined in the ECR session ‘Personalised radiology: myth or reality?’, which includes a presentation from renowned radiologist Professor Gabriel Krestin, chairman of the radiology and nuclear medicine department at Erasmus MC, University Medical Centre, Rotterdam, entitled ‘From personalised to precision imaging: the impact on clinical practise’.
Report: Mark Nicholls

ECR 2016 - Don't miss
Thursday 3 March, 8:30–10:00 a.m., Studio 2016 PC 5
Personalised radiology: myth or reality?
Speaking ahead of ECR, Professor Krestin told European Hospital: ‘Personalised medicine and personalised imaging means the customisation of the whole healthcare continuum tailored to the individual patients – it’s the right treatment to the right patient at the right time. In this context many radiologists would say radiology has always been personalised because what is more personalised than an image?’
To demonstrate this, he will offer six images showing very different diseases all manifesting with the same leading symptom - right lower quadrant abdominal pain. ‘The image gives a very personalised diagnosis, but also allows us to personally stage the disease and see how extended it is and which organs are involved and also to show whether the disease is homogenous or heterogeneous, where exactly disease is located and what structures are involved,’ Krestin explained. In this context imaging facilitates personalised treatment, with monitoring and adjustment, and optimal treatment choice and route of access for surgery. But that is taken a stage further with precision imaging.
Defined as stratification medicine, Krestin – awarded the Gold Medal of the European Society of Radiology at this year’s ECR – said it revolves around the idea that individual characteristics, molecular or otherwise, can improve medical research and daily practice.
‘For that, molecular methods and also imaging should be standardised, structured and quantitative and different types of information should be integrated,’ he said. ‘In this way quantitative imaging biomarkers have been developed, and validated, that can predict disease with high accuracy; you can measure the volume of certain brain areas and predict with a high probability the development of Alzheimer’s disease. These biomarkers are now translated from research into daily practice.’
Algorithms automatically measure brain structures volume
Personalised medicine and personalised imaging means the customisation of the whole healthcare continuum tailored to the individual patients
Prof. Gabriel P. Krestin
His team at Rotterdam has developed automated image processing algorithms that allow radiologists to measure accurately, using full automation, the volume of different brain structures, using dedicated work stations that calculate automatically these volumes and allow a clinician to see whether they are within the age-related norm or below, meaning that the patient has a relevant atrophy predicting the development of Alzheimer’s disease.
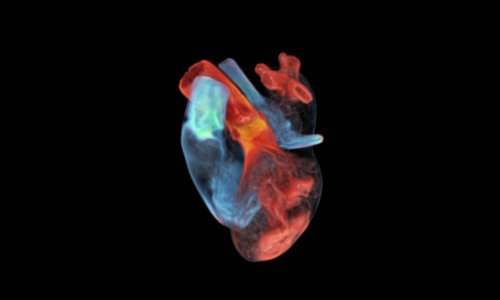
Another example is measuring coronary artery calcification as a strong prognostic factor for predicting those at risk of fatal coronary heart disease. Research has also shown great potential in the evaluation of therapy response of cancer patients by combining molecular information and imaging. Krestin believes this has already had an impact on daily practice.
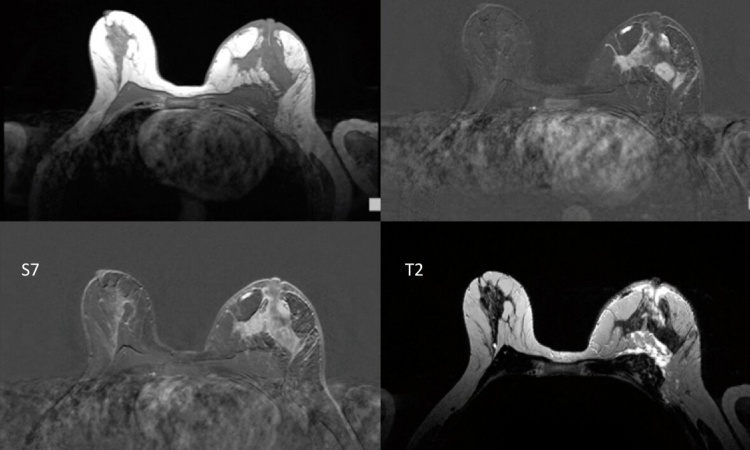
While RECIST is a recognised method for evaluating a certain lesion under cancer therapy, he believes more sophisticated ways of assessing response to treatment are already entering daily practice, either with nuclear medicine methods such as the metabolism of lesions with PET-CT, or looking to the perfusion of lesions with dynamic contrast-enhanced MRI.
He foresees more of these imaging biomarkers being validated and entering clinical practice with the combination of different diagnostic tools - not only for imaging but also molecular, biologic and biochemical tests - leading to integrated diagnostics.
Treatments will become more customised
An unselected use of very expensive drugs will be a lot more costly than the precise selection of those individuals who could benefit from a certain expensive treatment.
Prof. Gabriel P. Krestin
The evolution of a personalised approach combined with precision imaging will see fewer unnecessary treatments and side effects for patients. ‘The whole treatment will be a lot of more customised and, because we are using personalised prediction, it will help to identify, much earlier, those individuals who may be at risk of developing diseases.’
Krestin also believes the shift to personalised and precision medicine and imaging will be cost-effective. ‘An unselected use of very expensive drugs will be a lot more costly than the precise selection of those individuals who could benefit from a certain expensive treatment.’
Acknowledging that radiologists need more expertise in molecular biology, he suggests that they should also apply more measurements in their daily practice, because it is more accurate than descriptive reports. ‘Structuring reports, including quantitative data, is helpful in order to really compare results and deliver the relevant information to the clinicians,’ he suggested. ‘I also think integration of other relevant findings from pathology or laboratory medicine into the final report in the sense of an integrated report is the way forward.’
A range of imaging methods will still play a role because each has benefits and drawbacks and many are complimentary, depending on whether radiologists want to ‘predict, screen, make a diagnosis or monitor therapy’. Machine learning and Big Data will help manage the enormous amount of data and support the clinician in measurements, he said, as ‘perception with only the eyes will not reveal all the subtle findings. Some of these measurements are time-consuming, therefore algorithms based on machine learning and big data will help us to perform these relevant measurements in an automated or semi-automated fashion.
‘Big data will allow us to establish correlations between our imaging biomarkers and other “omics” information, putting imaging into a crucial role of elucidating pathophysiology and assessing on an individual basis the relevance and extent of disease.’
Profile:
Gabriel P Krestin is full professor of radiology and chairman of the radiology and nuclear medicine department at Erasmus MC, University Medical Centre Rotterdam, NL. Graduated at the University of Cologne, Germany, he completed his residency in radiology in 1988 and was later appointed radiologist and head of the MRI centre at Zürich University Hospital, Switzerland, where he became associate professor of radiology and head of the clinical radiology service, before moving to his present position.
03.03.2016