Multiple sclerosis
CNS damages are more complex than believed
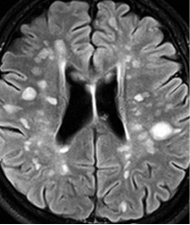
Multiple sclerosis (MS) – the inflammatory condition in the central nervous system (CNS) – leads to scarring, with several scars forming lesions, also called plaques. Although long assumed that only white matter is involved, this is increasingly questioned.
‘Today, it seems clear that multiple sclerosis is a diffuse disease of the CNS causing damages that are far more complex than previously thought,’ explains Professor Majda M Thurnher of the Clinical Department of Neuroradiology and Musculoskeletal Radiology at Vienna Medical University, speaking during a session on recent developments in MS research at the European Congress of Radiology (ECR 2013) in Vienna in March.
Magnetic resonance imaging (MRI) systems with higher fields, such as 3-Tesla or more, can detect relapse-caused lesions in grey matter. Particularly difficult to discover are juxta-cortical plaques, meaning those lying in-between white and grey matter. However, plaques can also form in the spinal cord as Prof. Thurnher explains: ‘Studies indicate that ninety percent of all MS patients show focal lesions in the spinal cord and that in thirty percent of MS patients the lesions are exclusively to be found in the spine.’ Spinal plaques are important because they allow an unambiguous diagnosis of the diseases.
‘Five to ten percent of patients below 50 years old show lesions in the white matter,’ explained Dr Frederik Barkhof, Professor of Neuroradiology at the Vrije University Medical Centre in Amsterdam (Netherlands). Those lesions, however, are caused by other pathologies, namely ischaemia associated with diabetes, hypertension or simply aging processes. They are restricted to the white matter and do not appear in the spinal cord. ‘If it is unclear whether a lesion in the brain is MS-related or ischaemia-related, take a look at the spinal cord,’ he advises. He believes a 3-T system is well suited and recommends T-2 weighted and proton-density weighted protocols.
MRI is a crucial modality not only in the initial MS diagnosis but also for therapy monitoring purposes. ‘New therapies particularly need to be closely monitored,’ he says. Case in point: Natalizumab is a drug that can significantly reduce inflammatory processes, lower the number of attacks and slow the disease. Unfortunately, 242 of the 96,000 patients who received natalizumab developed progressive multifocal leukoencephalopathy (PML), a potentially fatal viral infection that often occurs in immunosuppressed patients.
Eighty percent of all adults carry the JC virus, which the immune system usually keeps under control. While the clinical presentation of PML and an MS relapse are very similar, ‘MRI can distinguish PML lesions from focal MS lesions, which means PML can be diagnosed early,’ the neuro-radiologist explains.
MRI also allows earlier diagnosis of MS itself. ‘MRI shows the dissemination of the lesions in the brain and the spinal cord in time and space,’ the professor points out. In 2010, the so-called McDonald criteria to diagnose MS were revised and today the dissemination in time can be shown with a single scan he reports, adding: ‘This facilitates the diagnosis of MS.’
03.08.2013