MI treatment forbenign prostatic hyperplasia
An interview with Dr Andre Roggan, head of research and development at Celon AG, and Dr Markus Mueller, consultant at the Urology Clinic at the University Clinic Benjamin Franklin, Free University Berlin. Venue: 1st International Workshop on Radio-frequency Induced Thermotherapy (RFITT) for the treatment of BPH

EH: What is the difference between bipolar, radio-frequency induced thermotherapy or RFITT, as developed by Celon, and the conventional minimally invasive (MI) transurethral prostate resection with high-frequency resection loop (TUR-P)?
Markus Muller: TUR-P is the gold standard for the endoscopic treatment of benign prostatic hyperplasia, but this is not really a MI intervention. RFITT is not in direct competition with TUR-P, but it competes against other MI procedures - mainly in laser technology. Although the buzzword laser is very modern and mainly has positive connotations, there are disadvantages associated with laser procedures, which can be overcome with RFITT.
EH: What are the disadvantages?
MM: During a laser procedure, the surgeon gains little or no feedback from tissue and doesn’t know whether the dose used for tissue coagulation is actually sufficient. With RFITT, the great innovation is that, due to bipolarity, the equipment itself determines how long the coagulation procedure should last and can therefore be used with more precision.
The system has a function that measures the resistance of treated tissues as the current is applied. We know that this resistance correlates with the treatment’s progress, i.e. with the extent of the currently treated area. So the resistance is a direct benchmark for the therapy’s progress. During surgery, the system gives an acoustic feedback signal and the surgeon hears how the therapy progresses. At the end of the procedure, the machine switches itself of and gives the surgeon an acoustic signal - so he can be sure that tissue in the area where the equipment is currently being applied has been completely coagulated.
Apart from the acoustic signal, the temperature indicator, at the top of the probe, has another control function for the operator. The surgeon receives a direct feedback on the temperature development in the surgical area. The temperature is indicated on a monitor, in the operator’s direct field of vision, so the surgeon has twofold control during the whole operation.
EH: Very gentle for the patient...
MM: Yes, and - depending on a patient’s anamnesis - the procedure can also be carried out under local anaesthetic. Through optimum positioning of the flexible probe (puncture depth marking, temperature sensor and visual control) injuries and complications can be avoided.
EH: Could the temperature rise too far?
MM: Not at all! This is usually a problem in laser therapy when the length of application is based on previous experience. Too much laser and the tissue carbonises, so not enough energy gets into the tissue, which means that not enough tissue has been removed. This cannot happen with RFITT, because we can apply therapy for precisely the right amount of time. It is more exact and much faster than laser therapy, and more comfortable for the patient, due to the shorter treatment time and less time spent under anaesthetic. All of which also makes things easier for the surgeon - and it’s more cost-effective because it takes less time for us to carry out the procedure.
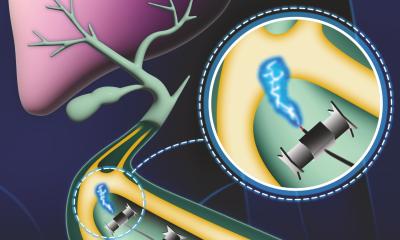
Andre Roggan: A further safety mechanism for the surgeon and patient is the performance and process regulation, which is independent of impedance and allows us to achieve reproducible coagulation figures. The system is characterised by its bipolarity - two electrodes, enabling current flow, are combined in one instrument. This means that electric current flows only in the precise area, and only this area heats up - as opposed to the classic HF surgical instrument with a single-pole connection. This means that the electric current flows through the whole body and can, in certain circumstances, cause vegetative irritations or burns near the conduction electrode. Single-pole HF technology cannot be used on patients with pacemakers - but our bipolar RFITT can be used without any problems.
EH: Are there further innovations for this technology in sight?
AR: There are always challenges. We can ask whether it is possible to reduce the number of necessary punctures; whether it will be possible to remove larger volumes in a shorter period of time, or whether efficiency can be increased to reduce operating times - less strain on the patient and lower costs. There is also the possibility that the procedure could be used in other medical fields.
We are already working on procedures for tumour treatment - the first probe for this is already in use, but not in urology. Another field will be ear, nose and throat (ENT) medicine. The probe used there is based on the same RFITT technology used to treat tumours - previously treated only palliatively. We also have projects based around liver metastases and liver tumours. So, we have a lot to do.
30.04.2003