Interview • Structured reporting
Liberating radiologists to be expert consultants
Where some decry the commoditisation of radiology, Gabriel Krestin MD, sees an opportunity to redefine the profession, for radiologists to rise up from basement reading rooms to consult as equals with other medical specialists in multi-disciplinary conferences focused on patient care. ‘If we are going to think about the future, we should not be looking in a rear view mirror. We need to be open to the changing environment,’ he said in this interview with European Hospital.
Interview: John Brosky

A past-president of the European Society of Radiology, Krestin will address the European Congress of Radiology on 5th March in a session dedicated to the future of radiology with his presentation entitled ‘Quo Vadis the Radiology Profession: A Pragmatic Approach.’ Professor Krestin spoke from his offices in Rotterdam, the Netherlands, where he chairs the Department of Radiology at the Erasmus Medical Centre.
What is your assessment of the state of radiology today?
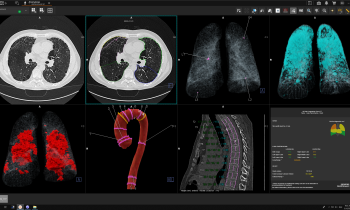
‘In this moment, when medicine is becoming more personalised for the patient, we are challenged to deliver greater precision. This definitely changes the face of radiology and the involvement of radiologists in the continuum of healthcare. What I want to talk about particularly is that this precision can only be obtained through standardisation, quantification, automation and integration. It means that we need a more structured reporting, which is quite obvious, but also a more extensive use of imaging biomarkers that means quantification of imaging characteristics.
Because we know that radiologists typically don’t like to measure, this will require a certain level of automated quantification in imaging. Coming around the corner are many algorithms in image processing and they are increasingly available where structures, functions and biomarkers that we consider important can be automatically quantified. If radiologists dislike measuring these things, automated processing will help them make reports more objective, more precise, and contribute to the concept of precision medicine.’
In this moment, when medicine is becoming more personalised for the patient, we are challenged to deliver greater precision.
Gabriel Krestin MD
Is the resistance to structured reporting due to the way it pushes against a tradition in radiology of interpreting images from an examination?
‘That is one of the reasons. A second reason is that it narrows the freedom to be more subjective, or to emphasise aspects you find of interest and tend to report more often. Structuring reports obliges a radiologist to go to a template each time and clearly and objectively report about every part of the exam. It obliges us to use more objective characteristics. It does not always need to be a number, but it does need to be a classification that is objective. This is what is meant by structure. It does not leave room for subjective descriptions where you are free to say something is ‘enlarged’. What can a clinician do with “enlarged”? Is it larger than five or seven centimetres? The clinician needs to know exactly what is meant by “enlarged”. Quantification and structuring go hand in hand.’
Structuring reports obliges a radiologist to go to a template each time and clearly and objectively report about every part of the exam. It obliges us to use more objective characteristics.
Gabriel Krestin, MD
Do you see the role of radiologists diminished?
‘Definitely not! We still have leverage, perhaps even more, because we will be taken more seriously. While there are measurements, and even if they become standardised, these measurements stay within radiology. ‘Two other issues that come in here; first, that the more an examination contains objective, measurable markers, the more it approaches other diagnostic specialties, such as pathology or laboratory medicine. A lab report, for example, delivers a long list of numbers of biomarkers measured in the blood or urine. My prediction, which is perhaps exaggerated and says exactly what radiologists would fear, is that our reports will look similar to lab reports, long columns of numbers, saying things like “At position N° 27 the number is 78”.
I don’t really believe our reports will ever look like that. Yet it is the direction we should be moving toward. My colleagues who are thinking in this way would love to have measures that are validated, consistent in delivering the same number no matter what technology is used. Like the creatinine value in blood, our measurements of, let’ s say the plaque volume in the coronary artery, should always be consistent and delivered as the same number.
We are very far away from this because industry is not really collaborating in this effort. We are far from standardisation in acquisition techniques. We are far from standardised processing techniques. We are far from being standardised in measurement techniques. We still have a long way to go. Yet this is where radiology, as a diagnostic specialty, needs to go, to be like laboratory medicine, moving toward reports that are open to integration – and this is the next topic – the integration between laboratory, pathology and radiology. Many people see this as the future of our profession. Integrating our diagnostic information with diagnostic information from other specialties to deliver a comprehensive report based on all these elements.’
Radiologists are still spending a lot of time producing these reports. Where the real added value of radiologists should be is in the multi-disciplinary conference where they can contribute to the management of the patient.
Gabriel Krestin, MD
In light of overwhelming utilisation of radiology today in every area of medicine, wouldn’t radiologists welcome the assistance of automation and standardisation to manage the sheer volume of the workload?
‘They should do so. In some healthcare systems, as is the case in the Netherlands and surely in many other countries, the product from the radiological service is the report, and less so the images. Radiologists are still spending a lot of time producing these reports. Where the real added value of radiologists should be is in the multi-disciplinary conference where they can contribute to the management of the patient.
Here, I tell my radiologists that if we have a shortage of staff with so much work to do, when we are forced to choose, it is better to postpone the reporting and get to the conference! This is where a radiologist should always be present as an adviser to consult with the primary care physicians and other specialists in deciding about the management of the patient.
This is my argument to address the fear some radiologists have about becoming obsolete because radiology is becoming commoditised. Already some aspects of radiology services are moving towards commoditisation. For example, scheduling of the examination can be out-sourced to a call centre or even utilisation management company. In most cases, radiographers and techs already perform the acquisition task. Even the reporting can be sent to less expensive sources where radiologists dictate reports of a sufficient quality.
But what can not be out-sourced, and what will never be commoditised, is the added value of consulting by the radiologist in a decision-making process and participating in the management of the patient. It’s where a radiologist brings knowledge of the
technology, both for its benefit and limitations. To be the specialist who knows what a structured report and the numbers in that report mean, as well as their significance for the patient.
This is what we need to deliver, not just a report. To give other physicians an appreciation of the study and an understanding that goes beyond their own specialties. This is where radiologists should be going. It brings us out of the basement and reporting
rooms into the conference room and even closer to the patient.’
04.03.2015