Interview • Clinical practice
LC-MS/MS enters the medical laboratory
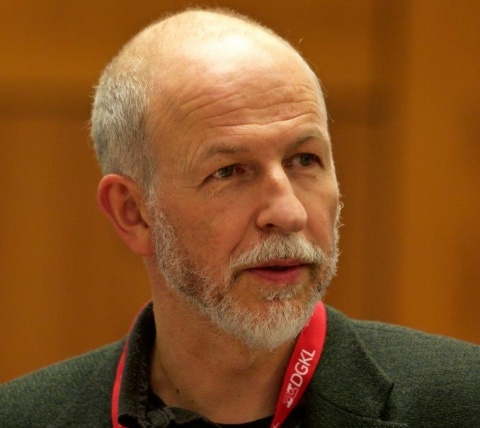
Over the last four years, Dr Thomas Stimpfl and his team have integrated mass spectrometry into routine analysis.
Interview: Walter Depner
The analytical technique liquid chromatography–mass spectrometry (LC-MS) combines the physical separation capabilities of liquid chromatography (or HPLC) with the mass analytical capabilities of mass spectrometry (MS). LC- and MS procedures were not originally developed for clinical/medical diagnosis; their introduction in the diagnostic laboratory has been problematic and taken longer than some had hoped. LC-MS, however, has already enjoyed notable success in Vienna and it is evident that this technology will be much more widely used in medical laboratories in the future. Our EH Correspondent spoke with Assistant Professor Thomas Stimpfl, head of Therapeutic Drug Monitoring and Toxicology at the Vienna General Hospital, about the implementation of the new LC/MS procedures.
Why was a largely non-medical analysis procedure introduced into the laboratory, and how long did that take?
Mass spectrometry, a standard procedure in forensics, was previously used for only a few specific analytes in laboratory medicine here. These analyses were complex, difficult to reproduce and prone to errors. Furthermore, only a few, select specialists in the field of biomedical analysis could carry them out. Making further developments in this field required much persuasion at all levels to prove the qualitative as well as economic superiority of mass spectrometry and its suitability for routine use. This is an on-going process and leads to a continuous expansion of parameters, which we determine via liquid chromatography–mass spectrometry.
LC-MS procedures need more technical application than conventional medical analysis. Was the staff affected?
In the beginning it was difficult for LC-MS to find widespread acceptance for the expansion of the parameter list. We had to use a lot of persuasion and some intensive training to familiarise staff with the more complex technology. Simplifications in handling and data evaluation, but also further developments of LC-MS systems towards classic medical analysers will make them easier to use in the future. Meanwhile, we now have 15 specialists in biomedical analysis in Vienna who can analyse the 85 LC-MS parameters independently (and also on weekends).

In your lab, which TDM parameters have changed to LC-MS/MS, and with what success? And which are also planned?
Immunosuppressants are now determined fully automatically via LC-MS, and this also includes aliquoting blood from the original sample tubes sent in. This step is essential for the repeatability of the overall process, since it has been observed that manual aliquoting of whole blood leads to significant variability. Moreover, after manual sample preparation, the same LC-MS systems are also used to determine psychopharmaceuticals, HIV-therapeutics, antiepileptics, antimycotics and cardiac agents. These analyses will soon be extended to antibiotics and endocrinological parameters. Its success lies in the enormous quality gain due to each sample now being given an isotope labelled, internal standard, and the current quality management, which is based on analytical batches, becoming focused on individual patients.
Which classic laboratory procedures – e.g. immunoassays (ELISA, RIA), photometry – have MS procedures replaced, or are some earlier procedures still used in parallel?
The development of a robust and easy to use LC-MS analyser will be key to extensive expansion of this new technology
Thomas Stimpfl
Immunoassays have been replaced, with the different analytic strategies to be viewed as complementary. In the future, qualitative and also economic factors will determine the use of the different technologies. Decisive for the success of LC-MS will be the automation of sample preparation, reliability and ease of handling of the analysers, complete LIMS integration and fast support from product specialists and service technicians.
The development of a robust and easy to use LC-MS analyser will be key to extensive expansion of this new technology, also enabling its use around the clock. As mass spectrometry can be used in very wide-ranging ways, this technology specifically lends itself to the establishment of new parameters and the closure of potential analytical gaps in the parameter spectrum.
What about the economic aspects of LC-MS?
The widespread establishment of LC-MS is still a challenge due to high costs involved (devices, laboratory adaptation), as well as the higher level of staff expertise required. In the long run, however, running costs will be lower, with higher flexibility and quality. The use of commercially available reagent kits offers a wide range of parameters. In our case this has led to a centralisation of services, where the University Hospital is now offering this service to hospitals throughout the city of Vienna. This also facilitates new financing concepts – such as including necessary analytical devices in the reagent kits and paying a price per reported result, which lowers the threshold for the establishment of LC-MS considerably.
Which systems do you use to achieve what capacities?
We use in-vitro diagnostic reagent kits from Chromsystems. The sample aliquoting and preparation for an annual total of 35,000 immunosuppressant determinations is carried out with a Hamilton device (as a batch) combined with Sciex mass spectrometers. The sample preparation for a further 15,000 LC-MS determinations a year is done manually because we don’t yet have the appropriate random-access automation. We are beginning to see some promising developments among some of the device manufacturers in this field.
New device/system/method integration into existing infrastructures is important in the modern laboratory; what happened in yours?
The minimum requirement in order to introduce LC-MS was defined as equivalence with the existing systems. Therefore, from the start, we aimed for the full automation of all processes and full integration into the LIMS; for instance there is no longer any manual data transmission. At the same time, we have been able to increase reliability and quality of results considerably.
Would you say the reliable and harmonic integration of MS into an existing diagnostic laboratory is a complete success?
We can say that mass spectrometry has been successfully established as a routine procedure in our laboratory. However, I believe this is only the beginning of an exciting development – we will see an increasing presence of clinical mass spectrometry in medical laboratories in the future.
Profile:
Assistant Professor Thomas Stimpfl PhD studied pharmacy and earned his doctorate in forensic chemistry at the University of Vienna in Austria. He worked as a forensic toxicologist both in Vienna and at the University Hospital Hamburg-Eppendorf in Germany before he moved to the Division of Medical-Chemical Laboratory Diagnostics at the Vienna General Hospital – Europe’s largest university hospital. He also heads a GLP-certified LC-MS laboratory at the Medical University of Vienna.
05.03.2018