Knee replacements
Demanding design, sophisticated technique and constantly improved materials guarantee lasting osseo-integration, writes Norbert Kamps, consultant engineer for aid provision and medical technology in Germany

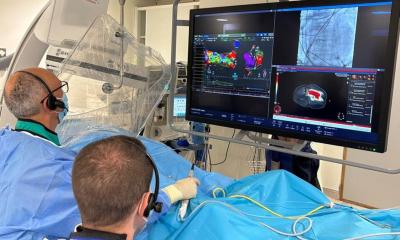
Replacing the function of human organs using exogenous materials has gained significance in recent years. In particular, there has been enormous progress in the technique of implanting artificial knee joints – knee endoprostheses – so that, with the development of new materials and prosthesis design, better results are being achieved. Durability of the prostheses has improved, while the rate of complications has dropped. Recent findings concerning reactions to foreign bodies and the biomechanical response in long-term use have led to many clinical studies of new materials.
An endoprosthesis used to replace a joint needs to not only withstand the natural physical load (compression, traction forces and shear stresses acting on it can amount to many times the body weight) but must guarantee the best possible replacement of the natural bone in terms of bone remodelling and mechanics. This is the precondition of osseo-integration, i.e. tolerable and permanent incorporation into the bony structures. Osseo-integration is determined by the design of the prosthesis, but the material of the prosthesis also plays a crucial role. There are therefore different models of knee replacements.
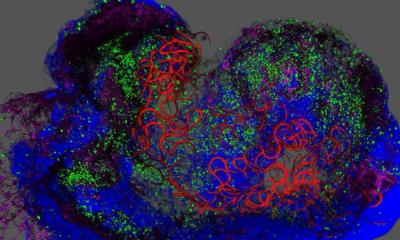
Bio-inert, bioconductive and bio-active materials are used depending on the form of strain and the area of use in the joint. Bio-inert materials, such as aluminium oxide or zinc oxide ceramics, are used for articulation surfaces. Bioconductive materials, such as titanium alloys, are used when bone accretion is desired. Bio-active materials, such as hydroxyapatite coatings (HA coating), are used for cement-free prostheses etc, since they ensure accelerated bony integration and thus a very solid bond. With metals (e.g. titanium, steel alloys), plastics such as PMMA (polymethyl methacrylate) or polyethylene are used. Today, the quality of the materials is defined in extensive regulations (e.g. ISO standards), but it may vary considerably between individual manufacturers. Abrasion and fatigue in particular are a major challenge to the materials used. Sliding and micro-movements lead to abrasion when the combination of materials is inappropriate and consequently to more or less severe complications caused by wear and tear. These reactions to foreign bodies essentially limit the present life expectancy of an endoprosthesis, so that this issue was, and still is, the focus of research and development. Today a large percentage of all aseptic loosening of prostheses is assumed to be due to reactions involving abrasion.
Knee replacements require optimised design, taking into consideration biomechanical demands, little bone loss, the simplest possible implantation technique and the least abrasion possible. Greater loading and improved life expectancy of the prosthesis were achieved by constantly enhancing materials. As a consequence the indication can be extended to ever younger groups of patients and quality of life can be increased. Another major challenge is the reconstruction of the damaged joint in as anatomically correct a manner as possible. New materials and optimised production techniques have opened up new perspectives here, as well.
Contact: hilfsmittel.kamps@arcor.de
30.10.2007