Credit: Patricio R. Sarzosa, Thayer School of Engineering
News • Power to the pacemaker
Harvesting the heart's energy to power life-saving devices
The heart's motion is so powerful that it can recharge devices that save our lives, according to new research from Dartmouth College.
We're trying to solve the ultimate problem for any implantable biomedical device
John X.J. Zhang
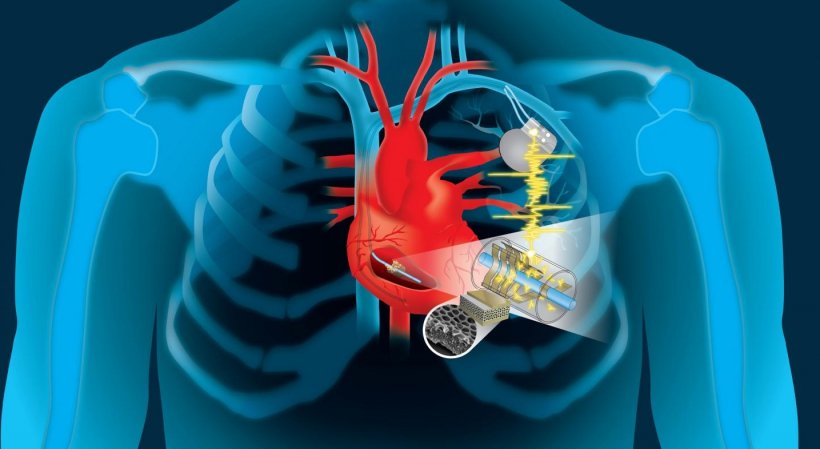
Using a dime-sized invention developed by engineers at the Thayer School of Engineering at Dartmouth, the kinetic energy of the heart can be converted into electricity to power a wide-range of implantable devices, according to the study funded by the National Institutes of Health. Millions of people rely on pacemakers, defibrillators and other live-saving implantable devices powered by batteries that need to be replaced every five to 10 years. Those replacements require surgery which can be costly and create the possibility of complications and infections. "We're trying to solve the ultimate problem for any implantable biomedical device," says Dartmouth engineering professor John X.J. Zhang, a lead researcher on the study his team completed alongside clinicians at the University of Texas in San Antonio. "How do you create an effective energy source so the device will do its job during the entire life span of the patient, without the need for surgery to replace the battery?"
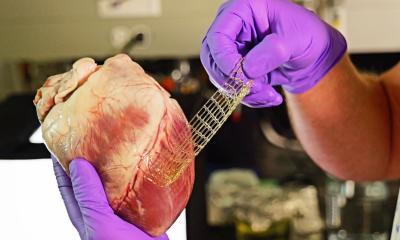
"Of equal importance is that the device not interfere with the body's function," adds Dartmouth research associate Lin Dong, first author on the paper. "We knew it had to be biocompatible, lightweight, flexible, and low profile, so it not only fits into the current pacemaker structure but is also scalable for future multi-functionality."
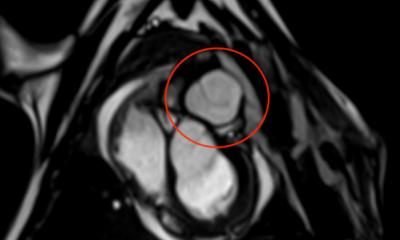
The team's work proposes modifying pacemakers to harness the kinetic energy of the lead wire that's attached to the heart, converting it into electricity to continually charge the batteries. The added material is a type of thin polymer piezoelectric film called "PVDF" and, when designed with porous structures -- either an array of small buckle beams or a flexible cantilever -- it can convert even small mechanical motion to electricity. An added benefit: the same modules could potentially be used as sensors to enable data collection for real-time monitoring of patients.
The results of the three-year study, completed by Dartmouth's engineering researchers along with clinicians at UT Health San Antonio, were just published in the cover story for Advanced Materials Technologies. The two remaining years of NIH funding plus time to finish the pre-clinical process and obtain regulatory approval puts a self-charging pacemaker approximately five years out from commercialization, according to Zhang. "We've completed the first round of animal studies with great results which will be published soon," says Zhang. "There is already a lot of expressed interest from the major medical technology companies, and Andrew Closson, one of the study's authors working with Lin Dong and an engineering PhD Innovation Program student at Dartmouth, is learning the business and technology transfer skills to be a cohort in moving forward with the entrepreneurial phase of this effort."
Source: Dartmouth College
05.02.2019