Glucose monitoring: from lab to POC?
Christian Pruszinsky reports
According to estimates up to 450 million patients will suffer from diabetes in the year 2025 (currently 250 million). In view of this, glucose monitoring is of utmost importance. Scientific studies and practical experiences with glucose monitoring at the point of care (POC) were evaluated recently during a meeting of experts in
Vienna.
Participants looked at POC glucose monitoring from many different angles: IT requirements, implementation
methods, effects on staff daily workloads, equipment specifications, industry supports, cost analysis, process
optimisation and best practices. Discussing the results of a study on process optimisation of glucose monitoring at fifteen selected hospitals in Germany, Switzerland and Austria, Professor Wilfried von Eiff, Director of the Centre for Hospital Management at Munster University, Germany, said: ‘Point of care testing is no all-purpose weapon but an indispensable element of any patient-oriented healthcare institution.’ The major advantage of POCT is time: within seconds results are available, in a ward, emergency department or out-patient clinics. Diagnostic and treatment measures can be initiated immediately and the data stored digitally.
Speaking with our Austria correspondent H C Pruszinsky, Prof. von Eiff, emphasised that POC glucose monitoring in a hospital makes sense in terms of quality and economy: ‘The number of diabetics is constantly increasing. The costs incurred by those who are ideally managed are only one eighth of the costs incurred by patients with poor disease management. Above all: patients with little fluctuation in blood glucose levels have the best long-term prognoses regarding sequelae, such as myocardial infarction, stroke, amputations etc. ‘Hospitals dealing with a high percentage of patients who need quick diagnoses, that is those with busy emergency departments, will
benefit most from POC testing. But hospitals or institutions with a decentralised structure and spatial layout are also well suited because long trips to the central lab can be avoided.’
Prof. von Eiff agreed that there is a potential conflict when tasks previously performed by the central lab are moved to wards. "POCT transfers tasks and responsibilities from the lab to nursing. Therefore, when restructuring the task portfolios the fact that nursing has to assume additional responsibilities must be considered. My viewpoint is that nursing is where the task of glucose monitoring should be performed. Obviously, hospital management has to ensure that nurses receive proper training, not only in the technology but also regarding the disease itself.
‘Nurses are increasingly “integrated caregivers”, diabetes managers so to speak. They will even decide which insulin doses are required or which measures can be suspended – to the extent obviously that no further special training is required to take these decisions.’ Laboratory workers do not fear layoffs, he agreed. ‘The areas of application of POCT are rather limited: for example, diagnostics that require fast results, in the emergency department or in the ICU. Lab staff is needed for calibration tasks and must continue with all those tests that need to be performed in the lab for quality assurance.
‘The biggest advantage of POC testing is time. Within seconds a diagnosis can be made and a therapy initiated. A disadvantage is that POCT means moving tasks from the lab to other departments. These changes should be clearly communicated and need excellent change management, involving informing the staff, convincing them, training them and arranging a user service for the staff performing the POCT. Are there possible cost savings? ‘Some, but nothing substantial; the major advantage of POCT is not financial but the fact that hospital safety and thus patient safety increase.’
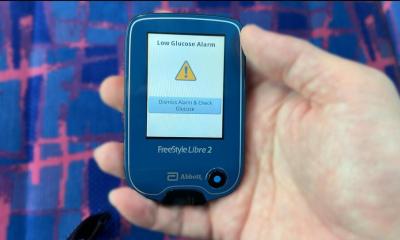
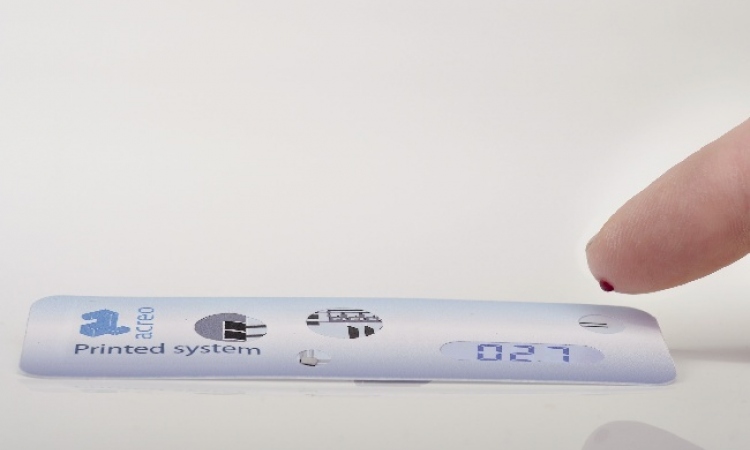
Blood glucose monitoring at the POC
Prior to each blood glucose test, the patient’s ID number is recorded by the POC glucose meter via a barcode reader. After the test, the device is placed into a docking station. From there the data –ID, test values and additional data such as date, time, device serial number, user ID and comments – are fed into the hospital information system (HIS) or the lab information management system (LIMS) and then can be accessed from the ward terminal. The central lab staff also has access to these data. They document them, perform a quality check and store them. That means quality assurance procedures on the wards are significantly reduced because documentation and archiving are performed in the lab. POC glucose meters employ biosensor technology, which processes specific data on the biochemical composition of a sample in real-time.
25.01.2010