Electronic discharge reports
Better for patients and physicians
Hospitals that use electronic medical record systems can improve the process of discharging inpatients by implementing electronic reports instead of dictated ones. More information can be provided in a faster, more reliable manner to the patients' caregivers outside the hospital, Electronic discharge summaries standardize the format and content of patient records to primary care physicians at the critical time when patients are being transferred from in-patient to out-patient care. Peer-review studies have proven that timely delivery of comprehensive, yet easy to read records, can reduce the number of preventable adverse events that may happen to a patient due to insufficient discharge information. Report: Kerry Heacox, of i.t. Communications
The urban complex that comprises Northwestern Memorial Hospital of Northwestern University covers several city blocks in downtown Chicago. Its medical informatics department is one of the largest and most progressive in the USA. It is regarded as one of the ‘most wired’ hospitals in the country, and has been on the ‘Top 100 Most Wired’ list of the American Hospital Association eight times.
Northwestern University Hospital installed a Cerner Millennium electronic medical record and computerized physician order entry system in August 2004. This system recorded patient history and progress notes, but did not provide a method for creating discharge summaries or delivering them automatically to the physicians’ offices or clinics. So the hospital informatics team developed its own system.
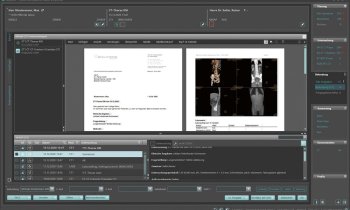
Physicians were surveyed to identify information they needed the most, and their requests were incorporated with national requirements to maintain accreditation. A patient discharge template was created. It was designed so that portions of the form would be automatically completed by the EMR, including patient demographics, lab results, and allergies and home medications. The electronic discharge system was activated in June 2006.
Elements of the discharge summary included date of admission and discharge, reason for hospitalization, discharge diagnosis, patient’s condition at discharge, and medications prescribed at the time of discharge. Patient history, exam summaries, significant findings of laboratory and radiology tests, pathology and stress test reports, and a list of procedures performed are included. The discharge summary also notes what tests do not yet have results, and lists follow-up issues of which the physician must be aware.
Once a discharge report is electronically signed, the system identifies the out-patient physician, or physicians treating the patient, and either electronically faxes a copy or sends it to a different EMR designated by the admitting physician.
In a formal evaluation of Northwestern’s patient discharge summaries before and after the hospital went electronic, a research team led by Dr Kevin J O’Leary, Associate Chief of the Division of Hospital Medicine, determined that the quality and clarity of the discharge summaries improved. Both reports were of similar length. With the electronic template, hospital physicians preparing the summaries could easily rank importance of the key results of lab and pathology tests and radiology reports. It was also much easier to indicate what test results were still pending, so that the patient’s doctor could follow-up to determine if any test results were abnormal.
One of the goals of implementing an electronic discharge record was to achieve 100% compliance that it would be completed within 72 hours after discharge. Even with electronic reminders to discharging physicians, only 75% initially complied. However, a comparative evaluation of 196 discharge reports showed that, in this sample, 72.6% of the electronic reports were completed within 72 hours, compared to only 59.4% using traditional paper forms.
The format of the electronic form is published in the online version of the April 2009 issue of the Journal of Hospital Medicine.
01.05.2009