News • AI, IT, data management
Digital attack on cancer
Several research groups at Berlin Institute of Health (BIH) are working on digitally combating cancer. The main goal is to combine and jointly evaluate existing information.
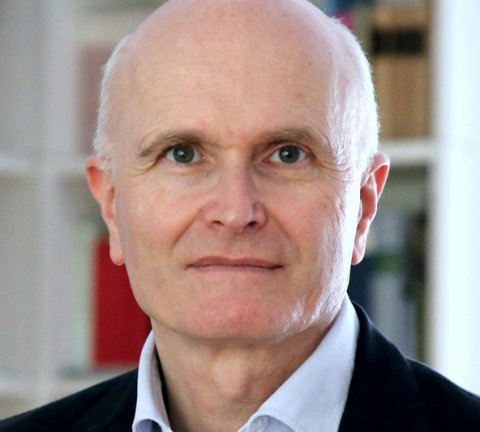
Image: Frederick Klauschen
With 500,000 new cancer cases every year in Germany alone, it is worthwhile comparing experiences with different diagnostic and treatment methods, thus allowing more patients to benefit from the most promising approaches. In addition, the BIH Digital Health Accelerator is helping innovators at Charité – Universitätsmedizin Berlin and the Max Delbrück Center to quickly bring digital ideas for cancer medicine to patients. “We welcome the initiative of the German Federal Ministry of Education and Research in declaring the National Decade Against Cancer,” says Professor Axel Radlach Pries, Dean of Charité – Universitätsmedizin Berlin and interim Chairman of the BIH Executive Board. “In the fight against cancer, we have placed a conscious focus on digitalization at BIH. Although we are increasing our knowledge about cancer every year, we need AI, IT, and data management specialists to evaluate the information and transfer it to clinical practice. For this reason, we have brought several researchers from these fields to the BIH who will support physicians and scientists at Charité and the MDC.”
Enormous wealth of experience must be tapped into

“We have a wealth of experience in Germany in treating cancer patients,” says Professor Sylvia Thun, head of the BIH eHealth & Interoperability Core Unit, which is supported by Stiftung Charité. “All we have to do is tap into it! But that’s not easy. The data of patients who provide information about their diagnoses, treatments, and disease progressions are recorded differently in each hospital. They are formulated differently and stored in various software systems, or even on paper. “It is therefore not possible, for example, to compare the data of all breast cancer patients or all prostate cancer patients,” laments Sylvia Thun. This comparison could make it possible, for example, to find the most effective treatment for a rare genetic modification or a specific form of prostate cancer. Or help to prevent severe side effects of the medications used by selected patients.
Communication standards in healthcare
“We need communication standards in healthcare,” says the physician. “This is why we have systematically set about processing data from molecular biological findings, tissue and blood tests, as well as the oncological reports that provide information on the type of tumor and what stage the tumor is at. This requires physicians to enter their diagnoses in a standardized “universal technical language.” “Naturally, this will initially be seen as extra work, but we hope that the physicians will soon sense the added value that this formalized input will bring.” And Thun and her team are going even further. In a next step, she would also like to introduce standards for transmitting data from smartphones. This should help make it possible for patients to regularly send information about their health status to their doctor so that he or she can see how successful the therapy actually was and how the patient is doing.
Combining data from healthcare and research

Professor Roland Eils is founding director of the BIH Digital Health Center and coordinates the medical informatics consortium HiGHmed, funded by the German Federal Ministry of Education and Research. The consortium connects medical faculties and university hospitals as well as medical technology and information technology companies from all over Germany. Eils’s aim is to combine data from patient care with data from basic biomedical research. Progress in research now makes it possible to track and analyze individual cells in the body. In this way, scientists and doctors can obtain information about the disease process in unprecedented detail. However, these enormous quantities of data, which are generated solely during the genome sequencing of cancer patients, must be digitally processed and combined with data from patient care before they can be used for personalized therapy. “This is the only way we can gain insights into what a specific change in the genetic makeup ‒ a mutation ‒ actually means for the cancer being treated,” explains Eils.
Digital bridge between hospitals and research
“Here at BIH, we’re trying to build a bridge between these two data landscapes.” Eils sees the added value of such a bridge for both sides. “On the one hand, of course, we are making a contribution to improving patient care through research. And on the basic research side, we benefit from seeing how our findings are implemented in healthcare and what results they bring patients. Only in this way can we understand the extent to which our disease models, which we utilize in basic research, are suitable for patient applications.” In order to link the data worlds from research and clinical practice, Eils and his colleagues are developing methods and technologies that make data streams as transparent as possible for both the treating physicians and researchers.
Roland Eils is aware of the reservations that many patients have when it comes to sharing their health data. Many scientists are also reluctant to make their findings freely available. “Information technology offers technical solutions that address data privacy and security issues,” says Eils. “And so I’m assuming we can provide fresh momentum to overcome any restrictions that may arise due to data privacy and security concerns.”
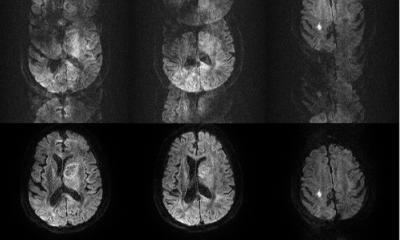
Digital diagnosis via artificial intelligence
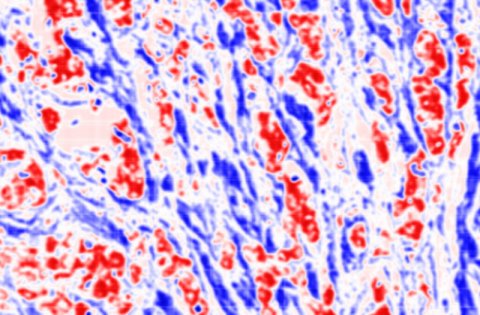
The usual way to determine if a suspicious lump is cancerous requires microscopic examination in a pathology laboratory. In order to ease the workload of pathologists who face a rising number of cancer cases and increasingly finer techniques for morphological and molecular diagnosis, Frederick Klauschen and his colleagues at Charité’s Institute of Pathology have teamed up with scientists led by Klaus-Robert Müller of TU Berlin to develop a digital imaging analysis system that uses artificial intelligence to evaluate microscopic images. “We pathologists are still superior to computers in performing a qualitative analysis, that is, when determining whether a tumor is malignant or not,” says Frederick Klauschen. “But when it comes to making quantitative statements, such as when determining what percentage of tumor cells contain a certain therapeutically relevant receptor, our digital system can provide valuable help because it is both faster and more precise.” Quantitative statements made during the diagnostic process are playing an increasingly important role in subsequent therapy. Patients will only receive the corresponding antibody therapy if, for example, the Her2neu receptor is detectable in at least 10 percent of tumor cells with a certain staining intensity. Or if a very large number of immune cells infiltrate the tumor, it probably makes sense to consider immunotherapy as well.

The software the researchers developed is already being tested in routine diagnostics at the Institute of Pathology. There are plans to conduct even more in-depth studies at other institutes and clinics before putting the technology into use. BIH supports innovators in translating their digital health projects into clinical practice. “In this particular case, we are helping to further develop the product and business model and to get the diagnostic software certified,” explains Tim Huse of the BIH Digital Health Accelerator. “We are also helping to commercialize the invention, either by collaborating with an industrial partner through an licensing arrangement or by starting a new company.” Physicians usually prefer not to be involved primarily on the business side, but want to continue to work mainly in a clinical setting. “We therefore also assist them with finding experienced co-founders with a background in either business or technology,” adds Huse.
Frederick Klauschen doesn’t believe that computers will completely replace him in the future. “Computers can perform very fast and precise calculations, but aren’t capable of learning without human help and can’t make clinical decisions either. So I don’t see the pathologist profession as being in any sort of danger. Roland Eils agrees: “Computers aren’t going to replace physicians. But physicians who use computers in their daily work will replace those who don’t.”
Source: BIH - Berlin Institute of Health
05.02.2019