Diagnosing brain tumours - stick to the standards!
As a referral neuroradiologist for paediatric tumour studies, Professor Monika Warmuth-Metz, Consultant at the Neuroradiology Department at University Hospital Würzburg, daily evaluates MRI images of different origin and colour. Her resume states: ‘All too often the standard protocols set out in the guidelines are not adhered to, which makes evaluation and follow-up significantly more difficult.’
What does constitute a good standard examination?
Monika Warmuth-Metz: 'Based on the consensus guidelines of the European reference radiologists on paediatric brain tumour studies and the AWMF guidelines, the imaging of brain tumours comprises a T2 image, a proton density-weighted or FLAIR image and T1 images before and after contrast medium application. The guidelines also state that a T2 image on its own, without proton and FLAIR image, is not considered sufficient, and that the axial plane is the standard. Furthermore, the guidelines stipulate that the examination must be comparable. Although the diagnosis in adults is normally histologically backed up, imaging still plays a vital role.'
Why are the guidelines so often ignored?
Monika Warmuth-Metz: ‘They are only recommendations, not prescribed protocols. Another reason is that the new sequences, which go hand in hand with technological progress, push the importance of a standardised examination into the background. It is, of course, important and right to use new procedures, but the standard examination should not be forgotten. For example, MPR sequences, i.e. T1 weighted, three-dimensional sets of data, are very popular at the moment. They deliver important information for the operational-navigational and radiation planning systems.
‘However, over and over again I see that this sequence is frequently used in alternation with a spine echo sequence. Unfortunately in this case, the signal intensities of both sequences are hardly, or not at all comparable. In other cases, we receive excellent examinations where all opportunities of functional imaging have been exhausted, but where the postoperative examination for the determination of the extent of the remaining tumour is missing. Consequently the entire examination or individual sequences have to be repeated to avoid a wrong assessment.’
Which differential diagnosis do you need for brain tumours?
Monika Warmuth-Metz:‘Basically, we have to differentiate between primary brain tumours and secondary brain tumours. Among the secondary tumours we have, for instance, meningioma and especially metastases, which make up the largest number of lesions.
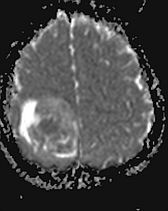
‘These days, due to the longer lifespan of cancer patients, the ratio between primary tumours and metastases is 50:50. With each mass in the brain– at least in adults – you have to think about metastases. With primary tumours in adults, the highly malignant, higher grade glioma tend to prevail. However, there are also non-tumourous changes that can perfectly imitate these images. This includes a brain abscess, which can easily be confused with cystic glioblastoma or cystic, highly malignant glioma.
‘Differentiation is carried out using diffusion weighting, i.e. the ADC image that shows a clear and homogeneous diffusion impairment in the case of abscesses. However, diffusion and ADC images respectively are also suitable for the determination of malignancy in glioma as indeed is the case of the more cells there are the higher the grade of malignancy.
‘Proton spectroscopy offers further options. It can be used to detect free lipids, which normally are not present in the brain and point towards necrosis. If a glioma is present that has free lipids, this image only really fits a necrotising, primary tumour, i.e. a glioblastoma.
‘Another, important differentiation is that of lymphoma, which are not primary brain tumours but haematological systemic diseases. However, they can present as images identical to those of higher grade, primary brain tumours. Differentiation is important here because primary lymphoma should, for instance, not be treated with corticosteroids prior to biopsy, as this makes the histological confirmation much more difficult.
Which aspects of the highly complex area of brain tumours and their diagnosis are important for radiologists in private practice?
Monika Warmuth-Metz:‘From my point of view, it’s less important to go into the subtleties of differential diagnosis. As radiologists in private practice carry out follow-up examinations it’s much more important to determine if and how these are being carried out in a comparable manner because the complete response evaluation and therapy planning are based on the results of a follow-up examination. Therefore, the message is: If something is being measured, then on a comparable basis, please. And the second message in this context is: Please don’t carry out follow-up examinations without full knowledge of the previous examinations and their sequences respectively. If this advice is being adhered to, we’ll actually have gained a lot.’
26.10.2011











