Image credit: Dr Jenny Bramley / Radii Devices Ltd.
News • Evidence-generated sockets
Data-driven designs to improve prosthetic legs
Tech provides personalized design using data from other fittings and scan of residual limb
The technology has been developed by Radii Devices and the University of Southampton, and the results of an NHS trial have been published in JMIR Rehabilitation and Assistive Technology. The study shows that below-the-knee prosthetic limbs designed using the new approach were as comfortable on average as those created by highly skilled prosthetists, but with more consistent results. Crucially, the new method generates a basic design instantly.
The real value of this tool is to give the prosthetist a starting design quickly, meaning they can spend much more of their time working with their patient on perfecting the more complex, personalised aspects of the design
Maggie Donovan-Hall
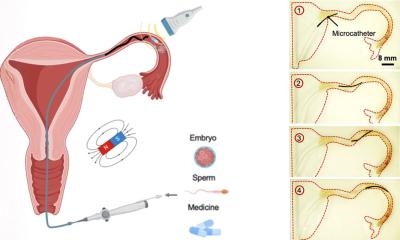
The team behind the software hope that data-driven ‘socket’ designs – the connection between the person and their prosthetic – will reduce the time, number of iterations and number of appointments it takes to arrive at a prosthetic limb the patient is comfortable with. This would not only improve patients’ experience but could also help to clear waiting lists.
Prosthetic sockets are personalised to make sure the prosthetic is comfortable, functional, and safe to walk on. The socket bears the person’s whole body weight and dynamic forces when walking, so it needs to be carefully balanced to distribute pressure without damaging limb tissue or creating discomfort. Traditionally, a prosthetist makes a plaster cast of the leg and reshapes it to produce a socket which achieves the right balance, producing trial versions before settling on a definitive one. Today, many prosthetists use CAD (computer-aided design) software in a similar way. Importantly, this creates a digital record of the design process, which the team were able to utilise.
Radii Devices Ltd, a spin-out company from the University of Southampton, has developed software which draws on data from previous prosthetic socket designs to generate recommendations for the most comfortable socket shape using a 3D scan of the patient’s residual limb. Dr Joshua Steer, Founder and CEO of Radii Devices and a co-author of the study, explains: “By analysing hundreds of previous prosthetic designs, we’ve been able to identify trends between different patient characteristics, such as the shape and size of the residual limb, and successful socket shapes. We can then scan a new patient’s residual limb and generate a personalised design recommendation based on features that have been successful for similar patients in the past.”
To test the effectiveness of the data-driven socket designs, the team carried out a study with patients from three NHS prosthetic rehabilitation centres. Seventeen patients were given a trial socket designed by a prosthetist and one designed using the new method. They were then asked to compare the comfort of the sockets, giving them a score out of ten, and interviewed about their experience of socket fitting.
The study found there was no difference in the comfort scores on average, and less variation in comfort in the data-driven socket designs. Several participants preferred the fit of the data-driven socket design when asked for feedback, and had it turned into their definitive prosthetic.

Image credit: Radii Devices Ltd.
The design recommendations aren’t intended to be used on their own in clinical practice. Instead, the team envision prosthetists working with the technology to further enhance the patient experience.
Alex Dickinson, Professor of Prosthetics Engineering at the University of Southampton, helped to develop the new method and the evidence base behind it. He said: “3D scans can tell us a lot about the shape of the residual limb from the outside, but they don’t tell us what is going on under the skin. Only a highly skilled prosthetist can identify things like bone spurs and neuromas, and know how to tweak designs to avoid causing pain or damage at these sensitive areas. We developed the data-driven socket design approach to save prosthetists’ time by giving them a solid base to work from so they can use their expertise where it is most valuable, in making precise adaptations tailored to their patients’ specific needs. The method effectively helps prosthetists to learn from each other.”
Nearly 100 people have now had a prosthetic leg designed this way, across multiple centres in the UK and the USA.
The project team included physiotherapists, health scientists, and software engineers. Maggie Donovan-Hall, Professor of Psychology in Prosthetics and Orthotics at the University of Southampton and co-author of the study, said: “This study was designed to test the ‘worst-case’ use of data-driven socket designs, with no additional input from prosthetists. The fact they performed so well in these circumstances is both surprising and encouraging, but the real value of this tool is to give the prosthetist a starting design quickly, meaning they can spend much more of their time working with their patient on perfecting the more complex, personalised aspects of the design. This is what prosthetists spend years learning and is most crucial to their patients’ experience.”
The final stage of this study is now underway, where the software interface is being developed with clinicians to provide them the most effective way to incorporate data-driven socket designs into their practice.
The work was supported by Innovate UK, the University of Southampton’s Institute for Life Sciences, Orthopaedic Research UK, and the Royal Academy of Engineering.
Source: University of Southampton
23.08.2025