Complementary cardiac imaging
The significant benefits of cardiac catherisation remain undisputed. However, cross-sectional imaging modalities are serious competitors when it comes to arriving at the right diagnosis.
‘The strength of CT lies in coronary diagnostics, the strength of PET in myocardial imaging. Both procedures complement one another in an ideal way.
‘In clinical practice we often see coronary pathology without perfusion defects and, vice versa, impaired coronary circulation without any visible damage to the coronary vessels. In these cases the complementary information from the PET/CT hybrid procedure is also very helpful.
‘With PET alone the perfusion of the heart muscle can be measured with various radiopharmaceuticals; however, it is also possible to examine the metabolism of the myocardium (glucose, acetate, fatty acids, for instance) or the myocardial innervation. Even infections (endocarditis, cardiac sarcoidosis, amyloidosis) can be diagnosed with the help of PET.’
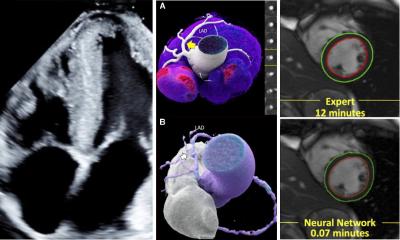
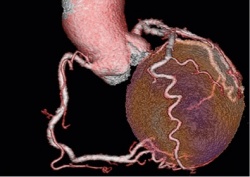
On the one hand, CT is used to improve the PET information in the sense of an attenuation correction, i.e. a purely technical measure. On the other hand, the CT data can be used to calculate the coronary calcium score. ‘The best discipline is the CT angiography, i.e. the visualisation of the contrast medium-filled coronary vessels and the quantification of the grade of stenosis,’ Hacker emphasises, and confirms: ‘The opinion now tends to be that if you have PET/CT available you should run the entire range of procedures, i.e. CT angiography plus PET perfusion measuring.’ Both procedures complement one another and thus deliver benefit.
Although PET perfusion measuring – with specificity and sensitivity of more than 90% – achieves a very high accuracy on its own compared to the more invasive coronary angiography, a simultaneous CT angiography additionally facilitates the attribution of any perfusion defects detected to the respective coronary stenosis that actually cause them. With PET alone, this can only be achieved in around 30% of cases. ‘This makes it possible to plan revascularisation measures,’ Hacker explains. Furthermore, first studies show that CT angiography also has an additional benefit regarding individual risk stratification of patients through the detection of coronary stenosis and non-calcified plaque deposits.
Computed Tomography angiography on its own is increasingly chosen as the first line examination to exclude coronary heart disease in patients with low to medium prior test probability for coronary heart disease. However, when the result of the CT angiography is not completely without pathological findings PET has significant additional benefits. ‘The positive predictive value of CT angiography to assess existing perfusion defects is very limited at around 30-40%.
When pathological changes in the coronary arteries can be seen, then CT angiography cannot predict whether these changes will lead to perfusion defects in the myocardium or not,’ Prof. Hacker explains. PET perfusion measuring is therefore the decisive criterion for treatment planning and risk stratification.
‘CT angiography with PET perfusion measuring facilitates complete, non-invasive, combined coronary-pathological and function cardiac diagnosis,’ he summarises, and predicts a great future for this hybrid procedure that has long moved on from its explorative stage. Unlike PET/MRI scanners, PET/CT scanners can be found in many facilities because of the oncological applications. Prof. Hacker: ‘PET scanners without CT are no longer even being manufactured.’
Profile:
Bavarian-born Professor Marcus Hacker has led the Clinical Department for Nuclear Medicine at the Medical University of Vienna since July 2013. Before this role the nuclear medicine expert was Head of Pre-clinical Imaging at the Clinic and Polyclinic for Nuclear Medicine, Ludwig Maximilian University in Munich.
02.09.2014