Cardiology roundup
The new £2 million remote access stereotaxis catheter laboratory at London's Heart Hospital, funded by the British Heart Foundation (BHF), is the first of its kind in the UK and one of only 40 worldwide.
New stereotaxis cath lab opens in London
The lab will enable doctors to perform angioplasty on patients at much higher risk of coronary artery disease and heart failure than previously possible at the hospital.
In traditional labs, the cardiologist stands next to the patient manually ‘pushing’ the catheter around the body. The new lab uses magnetic technology similar to an MRI scanner, and magnetic tipped catheters or probes are ‘pulled’ around veins and arteries by giant magnets operated with a joystick in a control room next to the theatre, allowing pinpoint precision. Professor William McKenna, clinical director of the Heart Hospital, said: ‘Currently, during complex electrophysiology and device procedures, it may take several hours to position the catheters. The new stereotaxis equipment will greatly improve our efficacy in such cases and be better for both patients and staff.’
Benefits include:
- As a result of quicker treatments (a 25% reduction in procedure time for complex electrophysiology ablation) patients are exposed to less radiation.
- Fewer members of staff are needed to support procedures, and those who are will be exposed to less radiation because they work outside the equipment room.
- Because treatments are less invasive, hospital stays are briefer.
- Recovery times are also said to be quicker, and some cardiac patients have a better chance of cure.
World renowned Centre of excellence halts heart transplants
Heart transplants are inherently high-risk, complex and gruelling procedures performed on a small number of patients in a ‘last ditch’ attempt to save already weakened lives. Therefore, success in this area is still celebrated.
Pending an investigation into why mortality had risen to three times the national average among some patients undergoing heart transplants, this procedure has been suspended at the renowned Papworth Hospital NHS Trust, near Cambridge, a National Health Service (NHS) hospital, where about 1,500 heart transplants have been carried out since 1979. The hospital is only one of five hospitals that carry out heart transplants. It gained international recognition largely due to the pioneering work of world-renowned cardiac surgeon Professor Sir Magdi Yacoub, now retired but highly active on the world’s cardiology stage.
The Trust itself raised the alarm itself after a routine audit showed that, since the beginning of this year, seven out of 20 patients who had received a heart transplant died within 30 days of the procedure in the first ten months of this year. On average, only 10% of patients would be expected to die within that period. However, as Steve Bridge, the hospital’s CEO, pointed out: ‘We’ve been around 7%, so we are below the national average. We are talking comparatively small numbers but it was agreed it would be sensible for us to invite the Healthcare Commission to undertake an external review. If there are any improvements we will make them.’
The UK’s Department of Health asked the Healthcare Commission, the NHS ‘watchdog’, to carry out a preliminary review.
Papworth employs 10 surgeons. At the time of going to press, their records are being ‘closely examined’ and the results of the review, due in mid-November, are to be sent to the UK’s Chief Medical Officer.
Lung transplants and other cardiac procedures, including bypass surgery, will continue.
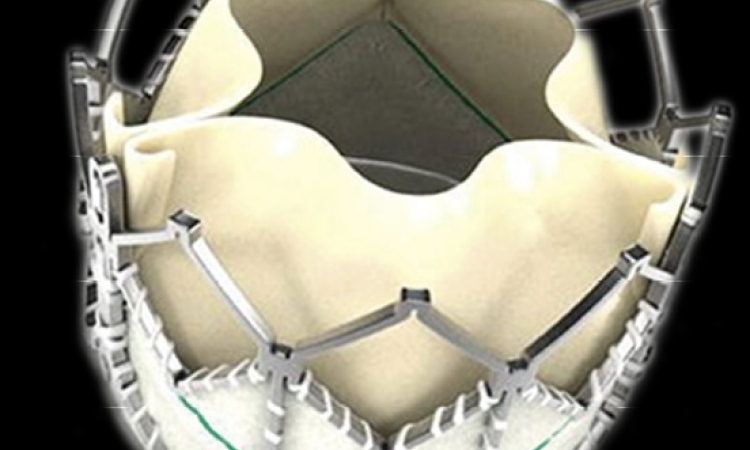
Proposed ban on drug-eluting stents
Angry cardiologists enter NICE discussions
Doctors are outraged by a proposal to ban the use of drug eluting stents (DES) currently used to treat some 30,000 patients annually – about 50% of all stent procedures – because the country’s National Health Service (NHS) has been advised by the National Institute for Health and Clinical Excellence (NICE) that drug eluting stents are not cost-effective.
Bare metal stents are about half the price of drug coated stents, which nowadays cost about £600.
Cardiologists have pointed out that diabetic patients or those with small blood vessels are more likely to suffer restenosis of arteries if given a bare metal device instead of the other. It could lead to a second operation and even a more expensive bypass.
Research in The Lancet medical journal has presented fresh evidence that using DES is not only cost-effective for high-risk patients, but also could save costs. In the study Swiss investigators carried out an 18-month observation of over 800 patients; two-thirds receiving DES; the rest, a bare metal stent.
Data on the diabetics involved, or those with small blood vessels, showed a 50% reduction in serious cardiac events, including second operations and heart attack, in those who received a DES. In addition, the death rate was lower in the DES group.
Overall, the researchers conclude that giving drug-coated devices to all heart patients is not cost-effective. But targeting the devices at high-risk patients is good value for money, the study concluded.
Not to be ignored: The researchers’ calculations for cost-effectiveness were similar to those used by NICE.
Cardiologists have estimated that at least 12,000 of patients given bare metal stents would need open heart bypass surgery in the future, due to the mentioned conditions, for example. They argue that bypass surgery is not only more expensive, but that the NHS could not cope with an estimated 50% rise in operations for patients unable to have stent procedures.
Professor Tony Gershlick, of the British Cardiovascular Intervention Society which opposes the ban, said the study confirmed what doctors had been saying to NICE: ‘We’ve never used drug-eluting stents for all patients and that isn’t what we’re calling for. Under current guidance, they are used in high-risk patients and this study shows they work well and are cost-effective because there is a 50% reduction in repeat procedures. Paying a small amount extra, which amounts to around £300 for each drug-eluting stent, is worthwhile for these patients.’ He also believes that NICE used out-of-date costing for drug- eluting stents, an early cost of £900 each. In addition, Nice had used only an audit from one hospital.
According to the BCIS, the proposed ban could cost the NHS an extra £60 million annually in surgery and re-stenting.
NICE is now discussing the ban, and a decision is expected before Christmas.
15.11.2007