Sponsored • Beyond average
A technological solution for preventing device-detected subclinical AF?
As pharmacological options for subclinical Atrial Fibrillation and atrial high-rate episodes continue to run into challenges, new research suggests more physiological pacing solutions can help reduce risks of progression to clinical AF.
One thing is clear. As common as subclinical atrial fibrillation is in patients with implantable devices, addressing subclinical AF (SAF) and atrial high-rate episodes (AHRE) remains a persistent challenge for even the most seasoned arrhythmia specialists.

Image source: Sander P et al., European Heart Journal 2024 (CC BY 4.0)
By themselves, oral anticoagulants are not improving overall outcomes for CIED patients with subclinical AF—at least if two big recent studies are anything to go by. Device-detected subclinical AF continues to be a significant risk factor for stroke and oral anticoagulants come with a higher risk of major bleeding. The European Heart Rhythm Association (EHRA) recently noted in its guideline updates that several controversies remain in treating AF—despite how common it is and how often new guidelines are published. Although anticoagulation is common, EHRA noted major discrepancies in how physicians manage bleeding risks.
While further advances in oral anticoagulation treatment may eventually clarify some of the controversies, what if researchers and industry could find a technological solution—within the CIED—to reduce subclinical AF and AHRE?
A new study suggests this is already happening.
Published in July’s issue of EP Europace, the recent Pisano et. al study followed 1,210 patients with sinus node dysfunction (SND) in 53 centers in Europe and Asia. About half of them had an implantable pacemaker or defibrillator with conventional accelerometer based DDDR pacing. The other half had devices equipped with Closed Loop Stimulation (CLS) —a pacing feature unique to devices from BIOTRONIK. After three years of follow-up, researchers found that the group of SND patients with dual-chamber CLS devices had a significantly lower AHRE incidence than the patient group receiving conventional accelerometer pacing.
Not only did the CLS group see a 16% reduced risk of subclinical AF and stroke risk, but the group also saw delayed onsets of AHRE – particularly ones that lasted a long time.

Clinical Benefits of the Closed Loop Stimulation in Sinus Node Disease (B3 Study)
Pisanò ECL, Calvi V, Viscusi M et al. Closed loop stimulation reduces the incidence of atrial high-rate episodes compared with conventional rate-adaptive pacing in patients with sinus node dysfunctions. Europace. 2024 Jun 28:euae175. doi: 10.1093/europace/euae175
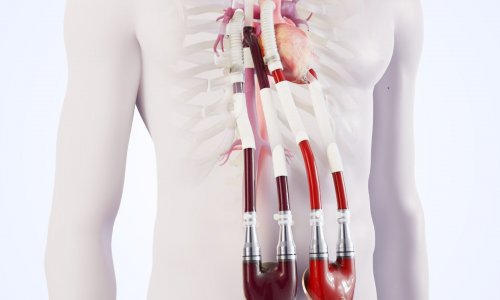
Image source: Biotronik
The physiological pacing difference – how CLS works to reduce AHRE risk
Instead of a conventional accelerometer, CLS features an impedance-based sensor with an algorithm that reacts to and adapts the pacing rate based on myocardial contractility.
This allows a CLS-equipped devices to react to mental stress as well as physical stress—with patients often remarking to their physicians about the positive effects CLS has on their quality of life. Depending on a patient’s profile, CLS’s unique pacing can provide clinical benefits as well—with CIED patients at risk of subclinical AF the latest to see these benefits backed up by fresh clinical evidence.
“Several studies showed integrating CLS into the autonomic regulation of cardiac output allows an effective heart rate modulation, restoring more physiological variability than an accelerometer sensor. We speculated this may have a beneficial effect in AF prevention, as previous smaller or retrospective studies indicated,” says Dr. Giovanni Luca Botto, Head of Electrophysiology at ASST Rhodense in Milan. “We designed and conducted a large RCT to definitively assess this hypothesis and provide a reliable estimation of such a benefit.”
Furthermore, in contrast to the increased risk of major bleeding that might accompany oral anticoagulation treatments, researchers did not observe CLS coming with any additional risk factors that might discourage its use in some patients.
What is next for addressing device-detected subclinical AF?
With 92% of physicians in one survey opting for anticoagulation treatment to deal with subclinical AF and AHRE, the need for more research into oral anticoagulation for CIED patients is obvious. Yet, whatever happens on the pharmacological side of the equation, the merits of a technological solution offering risk reduction without bringing in additional identifiable complications are clear.
“As clinicians look for additional options to prevent and manage atrial fibrillation in patients with a cardiac implantable electronic device, CLS offers the ability to better mimic normal sinus node function and proven to reduce subclinical atrial fibrillation,” says Dr. David Hayes, Chief Medical Officer at BIOTRONIK. In a field with plenty of controversy over how to prevent subclinical AF and AHRE in CIED patients, CLS offers an immediate chance to reduce those risk factors today—even as researchers look to the next clinical evidence the field needs.
With other similarly low-risk solutions hard to find in the field right now, CLS technology presents a great opportunity that is hard to ignore.
References:
- Pisanò ECL, Calvi V, Viscusi M, Rapacciuolo A, Lazzari L, Bontempi L, Pelargonio G, Arena G, Caccavo V, Wang CC, Merkely B, Lin LY, Oh IY, Bertaglia E, Saporito D, Menichelli M, Nicosia A, Carretta DM, Coppolino A, Ching CK, Del Castillo ÁM, Su X, Del Maestro M, Giacopelli D, Gargaro A, Botto GL. Closed loop stimulation reduces the incidence of atrial high-rate episodes compared with conventional rate-adaptive pacing in patients with sinus node dysfunctions. Europace. 2024 Jul 2;26(7):euae175. doi: 10.1093/europace/euae175. Erratum in: Europace. 2024 Aug 3;26(8):euae217. doi: 10.1093/europace/euae217. PMID: 38938169; PMCID: PMC11226787.
- Van Gelder IC, Rienstra M, Bunting KV, Casado-Arroyo R, Caso V, Crijns HJGM, De Potter TJR, Dwight J, Guasti L, Hanke T, Jaarsma T, Lettino M, Løchen ML, Lumbers RT, Maesen B, Mølgaard I, Rosano GMC, Sanders P, Schnabel RB, Suwalski P, Svennberg E, Tamargo J, Tica O, Traykov V, Tzeis S, Kotecha D; ESC Scientific Document Group. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024 Sep 29;45(36):3314-3414. doi: 10.1093/eurheartj/ehae176. PMID: 39210723.
- Sanders P, Svennberg E, Diederichsen SZ, Crijns HJGM, Lambiase PD, Boriani G, Van Gelder IC. Great debate: device-detected subclinical atrial fibrillation should be treated like clinical atrial fibrillation. Eur Heart J. 2024 Aug 3;45(29):2594-2603. doi: 10.1093/eurheartj/ehae365. PMID: 38935554; PMCID: PMC11297513.
- Boriani G, Gerra L, Mei DA, Bonini N, Vitolo M, Proietti M, Imberti JF. Detection of subclinical atrial fibrillation with cardiac implanted electronic devices: What decision making on anticoagulation after the NOAH and ARTESiA trials? Eur J Intern Med. 2024 May;123:37-41. doi: 10.1016/j.ejim.2024.01.002. Epub 2024 Jan 27. PMID: 38281819.
- Kommu S, Sharma PP. Subclinical Atrial Fibrillation: To Anticoagulate or Not? J Clin Med. 2024 May 30;13(11):3236. doi: 10.3390/jcm13113236. PMID: 38892946; PMCID: PMC11173250.
Source: Biotronik
05.12.2024