Image source: Empa
News • Smart wound sealing
Soldering wounds with light and nano thermometers
Not every wound can be closed with needle and thread. Empa researchers have now developed a soldering process with nanoparticles that gently fuses tissue.
The soldering technique is expected to prevent wound healing disorders and life-threatening complications from leaking sutures. The team recently published the promising method in the journal Small Methods and applied for a patent.
The idea of suturing a wound with a needle and thread dates back more than 5,000 years. Since then, this surgical principle has not changed much: Depending on the skill level of the person performing the operation and the equipment, cuts or tears in the tissue can be joined together more or less perfectly. Once both sides of a wound are neatly fixed to each other, the body can begin to close the tissue gap permanently in a natural way. However, the suture does not always achieve what it is supposed to: In very soft tissues, the thread can cut through the tissue and cause additional injury. And if the wound closure does not seal on internal organs, permeable sutures can pose a life-threatening problem. Researchers at Empa and ETH Zurich have now found a way to solder wounds using lasers.
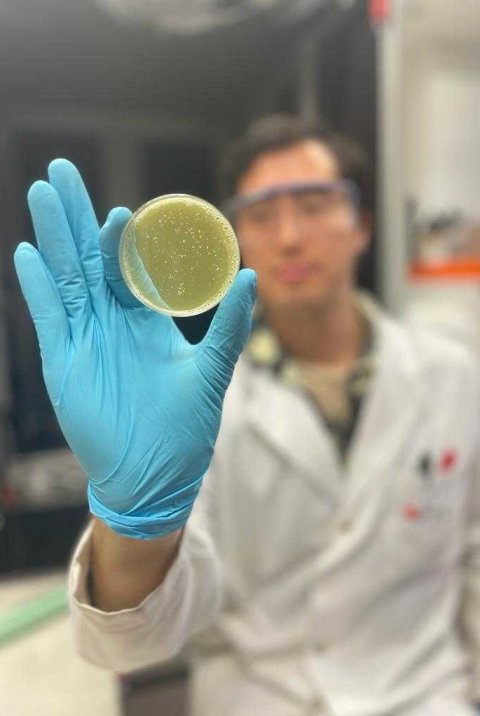
Image source: Empa
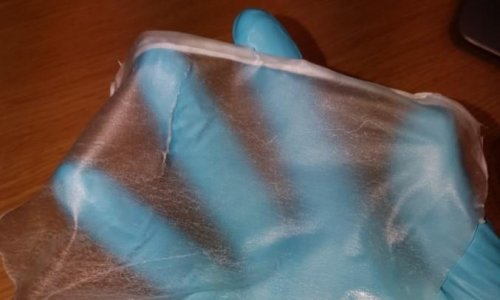
Soldering usually involves joining materials together by means of heat via a melting bonding agent. This thermal reaction must remain within narrow limits for biological materials, at the same time, the temperature is difficult to measure in a non-invasive way. This has been a problem for the application of soldering processes in medicine. The team led by Oscar Cipolato and Inge Herrmann from the Particles Biology Interactions laboratory at Empa in St. Gallen and the Nanoparticle Systems Engineering Laboratory at ETH Zurich therefore tinkered with a smart wound closure system in which laser soldering can be controlled gently and efficiently. For this purpose, they developed a bonding agent with metallic and ceramic nanoparticles and used nanothermometry to control the temperature.
The elegance of the new soldering process is also based on the interaction of the two types of nanoparticles in the bonding protein-gelatin paste. While the paste is irradiated by laser, titanium nitride nanoparticles convert the light into heat. The specially synthesized bismuth vanadate particles in the paste, on the other hand, act as tiny fluorescent nano thermometers: They emit light of a specific wavelength in a temperature-dependent manner, allowing extremely precise temperature regulation in real time. This makes the method particularly suitable for use in minimally invasive surgery, as it does not require stirring and determines temperature differences with extremely fine spatial resolution in superficial and deep wounds.
Once the team had optimized the conditions for "iSoldering" (intelligent soldering) via mathematical modeling in silico, the researchers were able to investigate the performance of the composite material. Together with surgeons from the University Hospital Zurich, the Cleveland Clinic (USA) and the Czech Charles University, the team achieved fast, stable and biocompatible bonding of wounds on organs such as the pancreas or liver in laboratory tests with various tissue samples. Equally successful and gentle was the sealing of particularly challenging pieces of tissue, such as the urethra, fallopian tube or intestine, using iSoldering. A patent application has now been filed for the nanoparticle composite material.
But the researchers didn't stop there: They succeeded in replacing the laser light source with gentler infrared (IR) light. This brings the soldering technology another step closer to be used in hospitals: "If medically approved IR lamps were applied, the innovative soldering technology could be used in conventional operating rooms without additional laser protection measures," says Empa researcher Inge Herrmann.
Source: Empa
16.01.2024